|
|
|
|
|
|
|
|
|
 Posted: Sun Jun 28, 2009 9:11 pm Posted: Sun Jun 28, 2009 9:11 pm
The ULTIMATE birth control information sticky, with all of the information you will ever need when researching birth control. 3nodding If there's something I'm missing, please use the Feedback Sticky and let me know.
I've used the names I'm familiar with up here in Canada. In other countries there might very well be something similar with a different name, but is in essence the same product, and so I might not have that variation listed. If you are using something similar to something I have listed, let me know and I will add the alternate brand name of the method in question.
I must apologize to everyone for taking so long to get to this! sweatdrop This has been on my to-do list for a VERY long time, and I'm happy I was finally able to finish it! heart
---
Table of Contents:
- Post 1: Introduction <--- You are here
- Post 2: The Pill
- Post 3: Ortho Evra Patch
- Post 4: Ortho Evra Patch - Additional and Supplementary Information
- Post 5: Nuva Ring
- Post 6: IUD (including info on Mirena)
- Post 7: Depo Provera (injection)
- Post 8: Depo Provera (injection) - Additional Information
- Post 9: Norplant (the implant in the arm)
- Post 10: Non-Hormonal Methods (diaphram, Lea Cup, spermicide, etc)
- Post 11: Why the Withdrawal Method is NOT An Effective Form of Birth Control
- Post 12: Birth Control: Choices and Chances [pamphlet]
- Post 13: Things That Interfere With Your Birth Control
- Post 14: Links and Resources [Phone numbers for people in BC, Canada only unless you're willing to call long distance]
- Post 15: Birth Control and Weight Gain
- Post 16: Effective Levels of Birth Control Brand For Each Method
- Post 17: Reserved.
- Post 18: Reserved.
|
 |
 |
|
|
|
|
|
|
|
|
|
|
|
|
 Posted: Sun Jun 28, 2009 9:20 pm Posted: Sun Jun 28, 2009 9:20 pm
The Pill(From the last sticky) The Pill - must be obtained by a prescription. - take one pill once a day. - complete one pill packet each month. - combination pills contain estrogen and progestin. - mini pills contain only progestin. - combination pills prevent release of the egg. - both types thicken cervical mucus to keep sperm from joining egg. Effectiveness: 97 - 99% effective - Not effective against STI's (STD's, but referred to as STI's in this pamphlet). Advantages: -nothing to put in place before intercourse, more regular periods. - less menstrual cramping, acne, iron deficiency anemia, premenstrual tension (PMS), rheumatoid arthritis. - protects against ovarian and endometrial cancers, pelvic inflammatory disease, non-cancerous breast tumors, and ovarian cysts. - fewer tubal pregnancies. Possible Problems: - must be taken daily. - rare but serious health risks, including blood clots, heart attacks and strokes --> women who are over 35 are at greater risk. - side effects include temporary irregular bleeding and other discomforts (such as nausea, etc). ----------------------------- Taken from: http://www.brown.edu/Student_Services/Health_Services/Health_Education/sexual_health/ssc/bcps.htm The Birth Control PillWhat are birth control pills?Birth control pills (BCPs) or oral contraceptive pills or have been used in this country for over 40 years. Safe and effective, they are one of the most extensively studied medications in the US The first birth control pill, Enovid, was introduced in 1960. Since then, over 45 brands have become available to women. BCPs have changed significantly since their introduction. Most importantly, the dosages of the pills have been markedly reduced. As the dosages have decreased, the side effects women experienced also decreased. Our currently prescribed pills have approximately one-tenth the amount of medication used in the first pills of the 1960's. How do BCPs work? Most BCPs contain two hormones: estrogen and progesterone. These hormones are synthetic versions of naturally occurring female hormones. They work primarily by preventing ovulation. There are 2 types of pill packs: - 28 day pill packs: 3 weeks of active hormone pills and 1 week placebo pills - 21 day pill packs: 3 weeks of active hormone pills only. Your period occurs each cycle, a few days after completing the active pills. Pills can be monophasic or triphasic. Monophasic means that the hormone pills all contain the same dosage. Triphasic pills contain slightly different amounts of hormone throughout the active pills. Monophasic and triphasic pills are equally effective and popular. How effective are BCPs in preventing pregnancy and STIs?BCPs are 98% to 99% effective for women who take the pills every day as directed. Pill-taking mistakes decrease effectiveness. There are detailed instructions on late or missed pills under the section -- How do I start taking BCPs? BCPs do not offer any protection against sexually transmitted infections (STIs).What are the side effects of BCPs?Like all medicines, BCPs have side effects that you need to be aware of. For BCPs, there are rare but serious side effects and minor side effects. Rare but serious side effects: Blood clotsBCPs can make women slightly more prone to form blood clots. A blood clot can occur in a vein or artery and can have different symptoms depending on where it forms. Clots can occur in the legs, abdomen, heart, lungs, eye, or brain. In the brain, a clot could manifest as a stroke. The risk of these events occurring is very low, but increases in women over 35, in smokers, and in those with high blood pressure, heart disease, diabetes, clotting tendency, or a family history of clotting abnormalities. The warning signs of a blood clot spell out the word ACHES: Abdominal pain Chest pain (also shortness of breath) Headaches (especially those that are new, severe, or associated with persistent dizziness, difficulty speaking, fainting,numbness or weakness in extremities Eye problems (blurred vision or loss of vision) Severe leg pain (and/or redness and swelling in the calf or thigh) If you develop any of the ACHES side effects or jaundice (a yellowing of the eyes or skin) while on BCPs, call Health Services right away. If you need emergency medical attention, call EMS. If you are out of town, contact a local health provider or go to a hospital emergency room. High blood pressureBCPs can raise your blood pressure. This is why we check your blood pressure a few months after you begin taking BCPs. Liver tumorsBCPs have been associated with an increased risk of forming benign liver tumors. This is a very rare occurrence, but you should contact your provider if you develop upper abdominal pain while taking BCPs. Breast cancer risk Many patients ask about how BCPs affect their future risk of developing breast cancer. The jury is still out on this issue. To date, there have been studies which suggest that there is a slightly increased risk of breast cancer in women who have used BCPs; however, breast cancer was diagnosed earlier and had a better prognosis than in women who have never used the pill. We encourage all women, especially those with a strong family history, to explore this risk with their provider. Cervical cancer risk The risk of developing this type of cancer is slightly increased in BCP users. Fortunately, routine Pap smear testing is an excellent screening tool and is recommended on a yearly basis for women taking BCPs. More common minor side effects of BCPs:NauseaSome women experience some mild nausea when first starting BCPs. Usually this goes away within a short time. Taking your pill with food or taking it before bedtime may help. If you have persistent problems or unusually severe nausea, contact your provider. Spotting or breakthrough bleedingThis is vaginal bleeding that occurs during your active pills. This is a very common side effect during the first 3 months of BCP use. Breast tendernessMild breast tenderness may occur after starting BCPs. The tenderness can be reduced by decreasing your caffeine and salt intake and by wearing a bra with good support. Usually it gets better within a few weeks. If you notice persistent discomfort or a discrete lump, make an appointment with your provider. Mood changes Some women may notice changes in their emotional status: depressed mood or emotional instability. If you have a history of depression, it is important to monitor your progress carefully when starting BCPs. If you notice changes in your mood after beginning BCPs, call your provider. Decreased sex driveWhile your sex drive is affected by many things, the hormones in BCPs can be a factor in decreased sex drive. If you are noticing this side effect, let your provider know. A change to another pill can improve this. Weight gainMany patients ask about this side effect. Studies have shown that weight changes in young women on BCPs are no different than women who don't take BCPs. Some women have noticed mild weight change (1 to 2 pounds) and mild fluid retention on some types of BCPs. Contrary to popular opinion, taking BCPs should not make you gain 10 or 15 pounds. Gallbladder diseaseBCPs may accelerate the formation of gallbladder stones in women who have a strong family history of gallstone disease. Cervical changes BCP usage, as well as pregnancy, have been associated with some cellular changes on the cervix, called a cervical ectropion. The delicate mucus secreting cells that line the inside of the cervix become present at the outer opening of the cervix. This can make the cervix more vulnerable to sexually transmitted diseases. Vaginal dischargeAll menstruating women have a cyclical vaginal discharge. BCP users may notice subtle changes, but most women won't notice any changes. What are the benefits of taking BCPs?- Regular cyclesBCPs are great at regulating the menstrual cycle, and this is especially helpful for women with periods that come too often or too infrequently. - Reduced menstrual crampsBCPs can offer significant relief to women with painful menstrual cramps. They also reduce the amount of blood flow during the period. Less blood loss is helpful in preventing anemia. - Reduced Acne We have known for years that BCPs can improve some women's acne. There are a few heavily marketed brands that are felt to be beneficial for acne. Some women have a marked improvement, others less. If this is a concern for you, discuss it with your provider. - Other important benefitsThe risk of developing benign breast cysts, ovarian cysts, pelvic inflammatory disease, and tubal pregnancy are reduced by taking BCPs. They also are associated with a markedly decreased risk of uterine cancer and ovarian cancer. Where can I get BCPs?For you to receive a prescription for BCPs, your medical providers will need to see you for a visit to take your medical history and perform an exam that usually includes a gynecological examination and Pap smear. If you have had such an exam within the last 12 months, you don't have to repeat it-but your medical provider will want to get a copy of the results. If you have never had a gynecological exam, call Health Services at 863-3953 to schedule an appointment. Let our staff know this is your first exam. The medical providers are very sensitive to and supportive of women having their first exams. The only charges during your visit will be for lab testing. You can choose to pay for any of our services directly if you don't want charges to appear on insurance bill or the Bursar's bill. After you and your provider choose a pill, you will probably receive a prescription for 1 month of pills with 2 refills. You will need to return for a brief appointment during the 3rd pack for medical provider to see how you are doing and to check your blood pressure. If you are doing well, you will be given a prescription to last 6 to 9 months. Women on BCPs should get a gynecological exam with a Pap smear once a year. The pharmacy in Health Services carries 5 to 6 types of birth control pills. The prices are at a reduced price, usually 50% cheaper than a regular pharmacy. You have the option of getting your pills at our pharmacy or at a local pharmacy. Some insurance plans cover BCPs, some don't. How do I start using BCPs?There are two ways to begin: - Sunday StartStart the first pill of your pack on the Sunday following the first day of your period. If your period begins Monday, Tuesday, Wednesday, Thursday, Friday or Saturday, start taking the pill that Sunday. If your period starts on a Sunday, begin taking your pill that very day. - First Day StartStart your first pill during the first 24 hours of your period. Be aware that during this first pack of pills, you will have two periods: one during the first week of pills and one on the fourth week of pills. After this first pack, you will get a period only once a month, on the fourth week of the pack, during the placebo pills. How long before the pill is effective?When starting BCPs, it will take 7 days for the pill to become effective at preventing pregnancy. You will need to use a second method of contraception during these 7 days. We recommend using condoms. In fact, we recommend using condoms consistently with BCPs to protect against sexually transmitted infections. Remember that BCPs offer no protection from acquiring STIs. Be aware that your first and last active pills are the most important pills in your pack. Being late starting your next pack or forgetting your last active pill will lengthen the time off the active pills. Lengthening this pill-free interval can allow your body to ovulate. Try to plan carefully when you need to start or purchase your next pack. Remember your pills when you go away for weekends or vacations. To help you remember to take your pill every day, it is useful to link taking your pill with some daily activity like brushing your teeth or eating a certain meal. Some women set a watch alarm to go off as a reminder. Each morning check your pack to make sure you took yesterday's pill. What if I'm late taking pills or I miss a pill?Taking your pill consistently every day gives you the best protection against pregnancy. Occasionally you may be late taking a pill or forget to take a pill. Spotting is likely to occur if you miss pills, but more importantly, the effectiveness of your BCPs can also be compromised. Here are some instructions to help enhance the effectiveness of your BCPs in those situations: - If you are less than 12 hours late for your pill, take it. You may wish to consider using a condom for the next 7 days, if you are not already consistently using condoms for STI protection. - If you forget 1 pill and 12 to 24 hours have elapsed since your last pill, take it as soon as you remember, then take your regular pill for that day at the same time you usually take it. Use condoms for the next 7 days. - If you forgot 2 pills in a row in the first 2 weeks, take 2 pills, 6 hours apart, on the day you remember, and 2 pills, 6 hours apart, the next day. Take 1 pill per day until the pack is finished. Use condoms for at least 7 days. - If you forget 2 pills in the 3rd week OR you miss 3 pills or more in a row at any time: - Sunday Starters Keep taking a pill every day until Sunday. On Sunday throw away the unused portion of the pack and start a new pack. Use condoms for at least 7 days. - First Day Starters Throw out the rest of the current pack and start a new pack the same day. Use condoms for at least 7 days. If you had intercourse without a condom during a time when you made a pill mistake, call Health Services to discuss whether you should consider emergency contraception. What should I do if I don't get my period?While your period may be much lighter on BCPs, you will get a period. Sometimes, however, no period occurs for a number of reasons: the low doses of the hormones, stress, or illness. If you've taken your pills regularly, pregnancy is unlikely. However, we do recommend taking a pregnancy test to rule out this possibility before starting your next pack of pills. We perform confidential urine pregnancy tests at no cost. If you aren't getting a regular period on BCPs, we may suggest a different pill. What if I lose a pill?If a pill is lost, you should replace it from a separate pack of pills. Call Health Services if this happens. Advice may vary depending on where you are in your pack and what type of pill you are on. What if I am vomiting or have diarrhea?If you vomit within two hours of taking your pill, you should consider that pill missed, and take another from a separate pack, as soon as you can keep things down. If you have 3 or more loose bowel movements for 2 days, the effectiveness of the pill may be reduced. We recommend that you abstain from sexual activity or use a condom for the duration of your illness and the 7 days afterwards. Can I skip a period on purpose?There may be a week when you would really like to avoid your period because of a special trip or event. You may accomplish this by not taking the placebo week of pills. Instead, throw them out and start your next pack of pills. Your period should hold off until you finish this new pack. This works a bit better with monophasic pills than with triphasic pills. We encourage women to try this only after they have been using BCPs successfully for a few months and have seen how their bodies adjust to BCPs. If you'd like to try this method, call your provider to discuss the details. What happens if I take antibiotics while I'm on the pill?We do know there are certain medicines that diminish the effectiveness of BCPs. The common antibiotics we use shouldn't affect the metabolism of BCPs. However, there have been some anecdotal reports by pill users who became pregnant while taking antibiotics. While the risk is very low, we encourage women to use condoms for the duration of their antibiotic prescription and for the following 7 days.What if I have breakthrough bleeding?Spotting or bleeding during the active pills of your pack is termed breakthrough bleeding. It is extremely common during the first three months of pill use. This bleeding can usually be ignored and should resolve by the third pack. If light bleeding persists for more than 5 to 7 days or heavy bleeding persists for more than 2 to 3 days, call your provider. We will sometimes recommend taking two pills a day (one it the morning, one in the evening) until the bleeding stops. The extra pills should be drawn from a separate pack of pills. Usually the extra pills need to be taken for 2 to 3 days. Breakthrough bleeding can also occur if you are late or forgot a pill. If you are experiencing breakthrough bleeding after your 3rd month of pill use for no obvious reason (you've taken your pills perfectly), you should call your provider. Do I need to stop using the pill from time to time?There is no evidence that you should "rest" your body from the pill periodically. It's generally not recommended to stop the pill unless you plan to stay off for 3 months. The best time to stop is at the end of your pack. Stopping during a pill cycle will usually be followed by some bleeding; count this as a menstrual period. Remember that you could become pregnant as soon as you stop taking the pills. However, your next normal period may be delayed. If normal menstruation does not return in 8 weeks, see your provider to determine why. Does the pill affect my ability to get pregnant later on?There is no evidence that BCP usage at any time is related to infertility. -------------------- All information taken from: http://www.wdxcyber.com/ncontr13.htmA very good site with information about the types of hormonal doses (estrogen and progestin) in each brand of the Pill, and information if you're looking to switch to another brand of birth control pill. Keep in mind the brands of Pill listed are taken from the website cited above, and not all brands are available in all places. I was put on Ortho - Tri Cyclen by my doctor, back when I was on the Pill, so if anyone wants any personal experiences with that brand, just PM me. smile Types/Brands of Birth Control Pills- Alesse. - Levlite. - Loestrin 1/2 FE (?) - Mircette. - Ortho - Evra (actually the patch, but it's listed on the website, so I'm adding it). - Estrostep FE. - Levlen. - Levora. - Nordette. - Lo/Ovral. - Desogen. - Ortho - Cept. - Loestrin 1.5/30. - Yasmin. - Triphasil. - Tri - Levlen. - Trivora. - Ortho - Cyclen. - Ovcon - 35. - Brevicon. - Modicon. - Necon. - Norethin. - Norinyl 1/35. - Ortho - Novum 1/35. - Demulen 1/35. - Zovia 1/35E. - Ortho - Novum 10/11. - Jenest. - Ortho - Tri - Cyclen. - Ortho - Novum 7/7/7. - Tri - Norinyl. - Necon 1/50. - Norinyl 1/50. - Ortho - Novum 1/50. - Ovcon - 50. - Ovral. - Demulen 1/50. - Zovia 1/50E.
|
 |
 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
 Posted: Sun Jun 28, 2009 9:27 pm Posted: Sun Jun 28, 2009 9:27 pm
The Ortho Evra Patch
(From the previous sticky)
Birth control patch
From MayoClinic.com
Special to CNN.com
The birth control patch is a 1 3/4-inch square, thin, beige-colored patch that you apply directly to the skin of your buttocks, abdomen, upper torso or upper outer arm. The patch continuously delivers two synthetic hormones, progestin (norelgestromin) and estrogen (ethinyl estradiol), which are similar to hormones your body produces on its own. The synthetic hormones impede pregnancy by preventing your ovaries from releasing eggs (ovulation). If eggs aren't released, sperm can't fertilize them and pregnancy can't occur. The patch also thickens your cervical mucus, making it difficult for sperm to enter the uterus and reach any eggs that may be released.
To help decide if the birth control patch is the best birth control method for you, find out how it works and how effective it is in preventing pregnancy.
How do you use the patch?
Use of the birth control patch is timed to coincide with your menstrual cycle. On the first day of your period or the first Sunday after your period begins, you apply the patch to your skin and keep it there for one week. On the same day each week for three weeks, you replace the old patch with a new one. The new patch can be placed on a different part of your body. During the fourth week, you don't apply the patch, and your menstrual period occurs. The following week you repeat the sequence.
If you don't start the first patch during the first 24-hours of your period, you must use an additional form of birth control for seven days to prevent pregnancy. If subsequent patches are applied and removed at proper times, additional birth control methods aren't necessary.
You can shower, bathe, exercise and swim while wearing the patch. Don't remove or change the location of the patch once you've applied it to your skin, as doing so may cause the patch to loosen.
In rare instances the birth control patch may loosen or fall off for other reasons. This usually occurs because the patch was applied incorrectly. To reapply a patch, press down firmly on the patch with the palm of your hand for 10 seconds, then run your fingers around the edge of the patch.
Don't reapply the patch if it's no longer sticky, if it has become stuck to itself or another surface, or if it has become loose or fallen off before. Don't use tape to keep the patch in place, and don't trim or alter the patch in any way. Doing so may alter the amount of hormones it delivers.
If you reapply the patch within 24 hours, its contraceptive effects remain intact. However, if more than 24 hours elapse, use an additional form of birth control until a new patch has been in place for seven days.
Are the effects of the patch reversible?
Yes. Once you go off the patch, you can get pregnant. But you may experience a delay before pregnancy takes place.
How effective is the patch at preventing pregnancy?
If you apply and remove the patch at the appropriate times each month, the patch is more than 99 percent effective at preventing pregnancy. Delaying or missing a weekly application or removing a patch too early can result in pregnancy.
Are any serious health risks associated with the patch?
Serious health risks are uncommon in healthy nonsmokers. Birth control patches have health risks similar to those experienced by users of oral contraceptives, such as a slight risk of blood clots in the legs or lungs and hypertension. If your doctor has advised you not to use oral contraceptives, he or she will probably advise you not to use the birth control patch, either.
Are there side effects?
Side effects associated with the patch are relatively minor and may include:
- Minor skin irritation at the application site
- Breast tenderness
- Headache
- Upper respiratory infection
- Menstrual cramps
- Abdominal pain or bloating
- Nausea
- Difficulty wearing contact lenses
Who shouldn't use the patch?
Don't use the patch if you smoke ? especially if you're over age 35, or if you have a history of:
- Migraines preceded by a visual disturbance, such as bright flashes of light
- Severe high blood pressure
- Diabetes with vascular complications
- Abnormal vaginal bleeding of unknown cause
- Blood clots
- Liver cancer or liver disease
- Breast or uterine cancer
- Heart attack or stroke
Does the patch help prevent sexually transmitted diseases?
No. The birth control patch does not protect against sexually transmitted diseases (STDs), such as HIV/AIDS, genital herpes and gonorrhea.
How much does it cost?
The initial medical examination costs between $35 and $125, according to the Planned Parenthood Federation of America. A monthly supply of birth control patches is similar to the cost of birth control pills ? between $15 and $35.
(Note: Keep in mind those are American prices, they will vary of course for Canadians or people from other countries.)
What's its availability?
The birth control patch is available by prescription only. At your initial doctor visit, he or she helps you determine if the birth control patch is an appropriate birth control option for you.
Advantages:
- Highly effective when used correctly.
- Doesn't inhibit sexual spontaneity.
- Minimal side effects.
- Contraceptive effects end shortly after you stop using it.
Disadvantages:
- Requires weekly application of new patch.
- Requires a prescription.
- No protection against STDs.
- Not for use by women who smoke or have certain health conditions.
- Must use another form of birth control for the initial seven days of use.
---------------------
(From the old Evra Patch Info Sticky)
Evra Patch Print-Out Info
This information is not intended to be comprehensive or replace the advice of your healthcare professional. Consult your healthcare professional with questions.
Ethinyl Estradiol/Norelgestromin Patch - Topical.
Warning: Smoking cigarettes/using tobacco while using this medication increases your chance of heart problems or stroke. Do not smoke. The risk of heart problems increases with age (especially in women over 35) and with frequent smoking (15+ cigarettes a day).
Uses:
This combination hormone patch is used to prevent pregnancy. It contains hormones similar to those in birth control pills (ethinyl estradiol, an estrogen, and norelgestromin, a progestin). The hormones slowly release from the patch over time and are absorbed through the skin. This medication works like birth control pills by preventing the release of an egg (ovulation) and changing the womb and cervical mucus to amke it more difficult for an egg to meet sperm (fertilization) or attach to the wall of the womb (implantation). Using this medication does not prevent you or your partner against HIV or other sexually transmitted diseases (STD's).
Studies have shown that the total amount of estrogen you receive when using the patch is higher than the amount from most birth control pills. If you weigh more than 198 pounds (90 kilograms), this patch may not work as well for you. Make sure your doctor knows your current weight, and ask about which form of birth control is best for you.
How to Use:
Read the Patient Information Leaflet provided by your pharmacist before you start using this medication, and each time you get a refill. Make sure you understand how to apply a new patch and dispose of the used product. If you have any questions, consult your doctor or pharmacist.
Remove the patch from the foil pouch and apply as directed by the manufacturer. Apply one patch to an area of clean, dry skin on the buttock, abdomen, upper outer arm, or upper body (torso) where it will not be rubbed by tight clothing. Change the patch once a week, and wear a patch continuously for 3 weeks or as directed byyour doctor. The change of becoming pregnant increases with incorrect use, so follow the directions carefully and make sure the patch stays in place.
Do not apply the patch on or near a breast, to red/cut/irritated skin, or over any other skin products (ie - make-up, lotions, powders, etc). Apply the patch to a different area on your body each time to avoid irritation.
If this is the first time you are using this medication, apply the patch on the first Sunday following the beginning of your menstrual period or on the first day of your period. If your period begins on a Sunday, begin on that day. For the first cycle of use only, use an additional form of non-hormonal birth control (ie - condoms or spermicide) for the first 7 days to prevent pregnancy until the medication has enough time to work. If you start the patch on the first day of your period, you do not need to use back-up birth control the first week. Change the patch once weekly on the same day. Remember to remove the old patch before placing a new patch.
After wearing patches continuously for 3 weeks, do not apply a patch during week 4. You should have your period during this time. If you do not get your period, consult your doctor. After not wearing a patch for a week, apply a new patch whether or not you have your period. Do not go longer than 7 days without a patch, or you will increase your risk of becoming pregnant. It may be helpful to mark a calander to remind you when to change the patch, and which week to leave it off.
If the patch comes off at the wrong time, replace with a new patch within 24 hours. If the patch is not replaced quickly, or if you are not sure how long it has been off, you could become pregnant. Start a new cycle by applying a new patch on the day you remember, and use an additional form on non-hormonal birth control (ie - condoms or spermicide) for 7 days to prevent pregnancy. Continue to apply patches for a total of 3 weeks.
After removing each patch, fold it in half so it sticks to itself, and discard it in the trash away from children and pets. Do not flush the patch down the toilet.
Ask your doctor or pharmacist for information from switching from other forms of birth control to the patch. If any of this information is unclear, consult the Patient Information Leaflet or your doctor or pharmacist.
Side Effects:
Vaginal bleeding between periods (spottin) may commonly occur during the first few months of use. If this bleeding is persistent or unusually heavy, contact your doctor. Nausea, vomiting, headache, redness/irritation at the application site, dizziness, breast tenderness/enlargement, vaginal discomfort/irritation, increased vaginal discharge, missed.irregular periods, acne, or stomach cramping/bloating may occur. If you miss 2 periods in a row (or 1 period if the patch has not been used properly), talk to your doctor about a pregnancy test. If any of these effects persist or worsen, notify your doctor.
Remember that your doctor has prescribed this medication because the benefit to you is greater than the risk of side efects. Many people using this medication do not have serious side effects.
Tell your doctor immediately if any of these unlikely but serious side effects occur:
- Change in vaginal bleeding (ie - continuous spotting, sudden heavy bleeding, missed periods).
- unwanted facial/body hair (hirsutism).
- Dark patches on the skin (leasma).
- Mental/mood changes (ie - depression, suicidal thoughts, persistent trouble sleeping).
- Sweeling of the ankles/feet.
- Weight changes (gain or loss).
- Problems wearing contact lenses.
This medication may rarely cause serious (sometimes fatal) blood clot problems (ie - thrombosis, pulmonary embolism, stroke, heart attack). Seek immediate medical attention if you experience:
- Tingling/weakness in the arms/legs.
- Pain/swelling/warmth in the groin/calf.
- Chest/jaw/arm pain.
- Confusion.
- Coughing up blood.
- Sudden shortness of breath.
- Sudden dizziness/fainting.
- Weakness on one side of the body.
- Vision problems/changes.
- Slurred speech.
- Sudden severe headaches.
- Headaches that are different from those you may have experiences in the past (ie - headaches with other symptoms such as vision changes/lack of co-ordination, existing migraines become worse).
Tell your doctor immediately if any of these highly unlikely but very serious side effects occur:
- Lumps in the breast.
- Severe stomach/abdominal/pelvic pain.
- Yellowing eyes/skin.
- Unusual tiredness.
- Dark urine.
A very serious allergic reaction to this drug is unlikely, but seek immediate medical attention if it occurs. Symptoms of a severe allergic reaction may include:
- Rash.
- Itching.
- Swelling.
- Severe dizziness.
- Trouble breathing.
If you notice other side effects not listed above, contact your doctor or pharmacist.
Precautions: (see also Warning section)
Before using this medication patch, tell your doctor or pharmacist if you are allergic to any of its ingredients; or to other estrogens or progestins; or if you have other allergies.
This medication should not be used if you have certain medical conditions. Before using this medicine, consult your doctor or pharmacist if you have:
- A history of strokes or other blood clots (ie - in the legs, eyes, lungs).
- Severe high blood pressure.
- Abnormal breast exams.
- Breathing problems (ie - asthma).
- Diabetes that has caused kidney/eye/nerve/blood vessel disease.
- Severe headaches.
- History of heart disease (eg - heart attack, chest pain).
- Heart valve disease.
- Kidney problems.
- Liver problems (ie - liver tumor).
- Current or suspected pregnancy.
- Seizures.
- Recent major surgery.
- Long periods of sitting or lying down (ie - immobility such as being bedridden).
- History of yellowing eyes/skin (jaundice) during pregnancy, or while using birth control pills.
- Unexplained vaginal bleeding.
- Heavy tobacco use (especially if over 35).
Before using this medication, tell your doctor or pharmacist your medical history, especially of:
- High cholesterol or triglyceride (blood fat) levels.
- Depression.
- Diabetes.
- High blood pressure.
- Fluid retention (edema).
- Gallbladder problems.
- Migraines.
- Obesity.
- Irregular/missed/very light periods.
- Recent pregnancy.
- Thyroid problems.
Do not smoke cigarettes. Hormonal birth control (ie - pills, injection [Depo Provera], devices [IUD]) products combined with smoking cigarettes significantly increases your risk for stroke, blood clots, high blood pressure, and heart attacks, especially in women over 35. For more details, ask your doctor or pharmacist.
Notify your doctor beforehand if you will be having surgery or will be confined to a chair/bed for a long time (ie - a long plane flight). You may need to stop this medication for a time or take special precautions in these circumstances while you are taking this drug.
The drugs in this patch may cause blotchy, dark areas on your skin (melasma). Sunlight may intensify this effect. If this occurs, avoid prolonged sun exposure, use a sunscreen, and wear protective clothing when outdoors.
If you are nearsighted or wear contact lenses, you may develop vision problems, or may have problems wearing your contact lenses. Contact your eye doctor if these problems occur.
This medicine patch should not be used in pregnancy. If you become pregnant or think you might be pregnant, inform your doctor immediately. If you have just given birth and are breast-feeding, or if you have had a pregnancy loss or abortion after the first trimester, wait at least 4 weeks before starting the patch. Talk to your doctor about other forms of birth control, and when it is safe to start the patch.
The medication from this patch passes into breast milk and may have undesireable effects on the nursing infant. Consult your doctor before breast-feeding.
Drug Interactions:
Your healthcare professionals (ie - doctor or pharmacist) may already be aware of possible drug interactions and may be monitoring you for them. Do not start, stop or change the dosage of any medicine before checking with them first.
This drug should not be used with the following medications because very serious interactions may occur:
- Amoratase inhibitors (ie - anastrazole, exemestane).
- Sodium tetradecyl sulfate.
- Troleandomycin.
If you are currently using any of these medications listed above, tell your doctor or pharmacist before starting this medication.
Certain drugs can decrease the effectiveness of combination-type birth control, by decreasing the amount of birth control hormones in your system. This can result in pregnancy. These drugs may include:
- Many antibiotics (ie - cephalosporins, chloramphenicol, macrolides such as erythromycin, penicillins, sulfas).
- Aprepitant.
- Bexaritene.
- Bosentan.
- Dapsone.
- Griseofulvin.
- Certain HIV protease inhibitors (ie - amprenavir, nelfinavir, ritonavir).
- Modafinil.
- Nevirapine.
- Rifamycins (ie - rifampin).
- Many seizure medications (ie - barbiturates, carbamazepine, phenytoin, lamotrigine, topiramate).
- St. John's Wort.
Consult your doctor or pharmacist for details, and ask them if you should use additional reliable birth control methods while taking any of the drugs mentioned above.
Before taking this medication, tell your doctor of all prescription and non-prescription medications you may use, especially:
- Acetaminophen.
- Ascorbic acid (vitamin C).
- Aspirin.
- Atorvastatin.
- Azole antifungals (ie - itraconazole, ketoconazole).
- Certain benzodiazepines (ie - diazepam, lorazepam, temazepam).
- Clofibric acid.
- Corticosteroids (ie - prednisolone).
- Cyclosporine.
- Metoprolol.
- Morphine.
- Phenylbutazone.
- Raloxifene.
- Tamoxifen.
- Theophylline.
- Medication for low thyroid (hypothyroidism).
This medication can affect the results of certain lab tests (ie - blood tests such as glucose, clotting factors, lipids, thyroid). Make sure laboratory personnel and all your doctors know you use this medication.
Overdose:
Overdose with this medication is highly unlikely. However, if overdose is suspected, remove the patch and contact your local poison control center or emergency room immediately. US residents can call the US National Poison Hotline at: 1 - 800 - 222 - 1222. Canadian residents should call their local poison control center directly.
Notes:
Do not share this medication patch with others.
Keep all laboratory and medical appointments. You should have regular complete physical exams including blood pressure, breast exam, pelvic exam, and screening for cervical cancer (pap smear). Follow your doctor's instructions for examining your own breasts, and report any lumps immediately. Consult your doctor for more details.
Missed Dose:
If the patch comes off, or if you forget to remove it at the proper time, consult the Patient Information Leaflet or your doctor or pharmacist to establish a new dosing schedule. You may need to use a back-up form of birth control (ie - condoms or spermicide) to prevent pregnancy.
If you have trouble remembering to change your patch, or if the patch falls off repeatedly, contact your doctor to discuss switching to another form of birth control.
Storage:
Store in protective foil pouches at room temperature at 77 degrees F (25 degrees C). Brief storage between 59 - 86 degrees F (15 - 30 degrees C) is permitted. Do not refrigerate or freeze. Protect from light and moisture. Keep all medicines away from children and pets.
-----------------------
(From the old Evra Patch Info Sticky)
Patient Information Leaflet
**The contraceptive patch DOES NOT PROTECT against sexually transmitted diseases (STD's), including HIV/AIDS. It is advisable to use condoms IN COMBINATION WITH the contraceptive patch.
The Evra contraceptive patch is a hormonal contraceptive. It contains two female sex hormones: 6.0mg norelgestromin and 0.60mg ethinyl estradiol in a thin, beige plastic patch that sticks to the skin. The sticky part of the patch contains the hormones norelgestromin and ethinyl estradiol, which are released continuously through the skin and into the bloodstream. Each patch is sealed in a pouch that protects it until you are ready to wear it.
Any woman who considers using the Evra contraceptive patch should understand the benefits and risks of using this form of birth control.
Hormonal contraceptives, including Evra have shown to be highly effective in preventing pregnancy when taken as prescribed by your doctor. Pregnancy is always more risky than taking hormonal contraceptives, except in smokers older than age 35.
This leaflet will give you much of the information you will need to make this decision, and will also help you determine if you are at risk of developing any serious side effects. It will tell you how to use the hormonal contraceptive patch properly so that it will be as effective as possible. However, this leaflet is not a replacement for a careful discussion between you and your healthcare provider. You should discuss the information provided in this leaflet with him/her when you first start using the Evra contraceptive patch, and during your revisits. You should also follow your healthcare provider's advice with regard to regular check-ups while you are using the contraceptive patch.
Who Should Not Use Hormonal Contraceptives
In general, hormonal contraceptives include birth control pills, injectables, implants, and the contraceptive patch [as well as the Nuva Ring]. The following information is primarily derived from studies of birth control pills. The contraceptive patch is expected to be associated with similar risks.
You should not use the Evra contraceptive patch if you have or have had any of the following conditions:
- Unusual vaginal bleeding that has not yet been diagnosed.
- Blood clots in the legs, lungs, eyes or elsewhere.
- A stroke, heart attack, or chest pain (angina pectoris).
- Known or suspected cancer of the breast or sex organs.
- Liver tumor associated with the use of the Pill or other estrogen-containing products.
- Jaundice or liver disease if still present, and/or
- Yellowing of the whites of your eyes, or of the skin (jaundice) during pregnancy or during use of hormonal contraceptives such as Norplant [the implant] or the birth control pill.
The Evra contraceptive patch should not be used if you are pregnant, or if pregnancy is suspected.
If you Decide to Use Evra
If you and your doctor decide that for you, the benefits of the Evra contraceptive patch outweigh the risks, you should be aware of the following:
1) Cigarette smoking increases the risk of serious adverse effects on the heart and blood vessels. The risk increases with age and becomes significvant in hormonal contraceptive users over 35 years of age. Women should not smoke.
2) Use Evra only on the advice of your doctor and carefully follow all directions given to you. You must use the contraceptive patch exactly as prescribed. Otherwise you may become pregnant.
3) Visit your doctor three months or sooner after the initial examination. Afterward, visit your doctor at least once a year.
4) Research suggests that the effectiveness of Evra may be reduced in women weighing more than 90 kg (198 lbs) compared with its effectiveness in women with lower body weights. If you weigh more than 90 kg (198 lbs), you should talk to your healthcare provider to determine which method of birth control may be right for you.
5) Be alert for the following symptoms and signs of adverse side effects. Call your doctor immediately if they occur:
- Sharp pain in the chest, coughing blood, or sudden shortness of breath. This could indicate a possible blood clot in the chest.
- Pain in the calf. This symptom could indicate a possible blood clot in the leg.
- Crushing chest pain or heaviness. This symptom could indicate a possible heart attack.
- Sudden severe or worsening headache or vomiting, dizziness, or fainting, disturbance of vision or speech, or weakness or numbness in an arm or leg. These symptoms could indicate a possible stroke.
- Sudden, partial or complete loss of vision. This symptom could indicate a possible blood clot in the eye.
- Severe pain or lump in the abdomen. This symptom could indicate a possible tumor of the liver.
- Severe depression.
- Yellowing of the skin (jaundice).
- Unusual swelling of the extemities, and/or
- Breast lumps. Ask your doctor for advice and instructions on regular self-examination of your breasts.
6) Hormonal contraceptives, including the Evra contraceptive patch should never be used if you think you are pregnant. Evra will not prevent the pregnancy from continuing. Check with your doctor about risks to your unborn child from any medication taken during pregnancy.
7) You will have a menstrual period when you stop using Evra. You should delay pregnancy until another menstrual period occurs within 4 - 6 weeks. Contact your doctor for recommendations for alternative method of contraception during this time.
8 ) Your doctor will advise you of the appropriate time to start the use of Evra after childbirth, miscarriage, or therapeutic abortion.
9) If you are breast-feeding, consult your doctor before starting the contraceptive patch. Hormonal contraceptives are passed on to the child in the milk. A few adverse effects on the child have been reported, including yellowing of the skin (jaundice) and breast enlargement. In addition, combination hormonal contraceptives may decrease the amount and quality of your milk. If hormonal contraceptives are not resumed until nursing is established, however, the quantity and quality of breat milk does not seem to be affected. If possible, do not use combination hormonal contraceptives while breast-feeding. You should use a barrier method of contraception sice breast-feeding provides only partial protection from becoming pregnant, and this protection decreases significantly as you breast-feed for longer periods of time. You should consider starting the contraception patch only after you have weaned your child completely.
10) Should you require major surgery, inform your surgeon that you are using the Evra contraceptive patch. You should consult your doctor about stopping the use of the contraceptive patch 4 weeks before surgery and not using the contraceptive patch for 2 weeks after surgery or during bed rest.
11) If you see a different doctor, inform him or her that you are using the Evra contraceptive patch. If you are scheduled for any laboratory tests, tell your doctor you are using the Evra contraceptive patch, since certain blood tests may be affected by hormonal contraceptives.
12) Inform your doctor if you are taking, or if you start to take other medications. This applies to both prescription and non-prescription drugs. These medications may change the effectiveness and/or cycle control of your contraceptive patch. You may need to use a back-up method of birth control.
Certain drugs may interact with hormonal contraceptives, including the contraceptive patch, to make them less effective in preventing pregnancy, or cause an increase in breakthrough bleeding. Such drugs include rifampin, drugs used for epilepsy such as barbiturates (ie - phenobarbital), anticonvulsants such as topiramate (ie - Topamax (c) ), carbamazepine, phenytoin. phenylbutazone, certain drugs used in the treatment of HIV or AIDS, and possible certain antibiotics. Tetracycline has been shown not to interact with Evra. A possible interaction has been suggested with hormonal contraceptives and the herbal supplement St. John's Wort based on some reports of oral contraceptive users experiencing breakthrough bleeding shortly after starting St. John's Wort. Pregnancies have been reported by users of combined hormonal contraceptives who also used some form of St. John's Wort.
As with all prescription products, you should notify your healthcare provider of any other medications you are taking. You may need to use a barrier contraceptive when you take the drugs that can make the contraceptive patch less effective.
13) There is no need to stop taking the Evra contraceptive patch for a "rest period".
How to Use Evra
Instructions for use.
The transdermal system keeps you from becoming pregnant by transferring hormones to your body through your skin. The patch must stick securely to your skin in order for it to work properly.
The system uses a 28 day, 4 week cycle. You will apply a new patch each week for 3 weeks - 21 total days. You will not apply a patch during week 4. You will have your period this week.
This means that every new patch will be applied on the same day of the week. The day will be your "Patch change day". For example, if you apply your first patch on a Monday, all of your patches should be applied on a Monday. You will wear only one patch at a time.
Save these instructions.
1) If this is the first time you are using the birth control patch, wait until the day you get your menstrual period. [Talk to your doctor if unsure, or if he/she tells you otherwise.] The day you apply your first patch will be Day 1. Your "Patch change day" will be on this day every week.
2) For a First Day start: apply your patch during the first 24 hours of your period.
or
For a Sunday start: apply your first patch on the first Sunday after your period starts. You must use back-up contraception for the first week of your first cycle only.
3) Choose a place on your body to put the patch. Put the patch on your buttock, abdomen, upper outer arm or torso, in a place where it won't be rubbed by tight clothing. Never put the patch on your breasts. To avoid irritation, apply each new patch to a different place on your skin.
4) Using your fingers, open the foil pouch by tearing it along the edge. Firmly grasp a corner of the patch and gently remove it from the foil pouch. Sometimes the patch can stick to the inside of the pouch - be careful not to accidently remove the clear liner as you remove the patch. Then peel away half of the clear protective liner. Avoid touching the sticky surface.
5) Position the patch on your skin, and then remove the other half of the liner. Press down firmly on the patch with the palm of your hand for 10 seconds, making sure that the edges stick well. Check your patch every day to make sure that it's sticking.
6) Wear the patch for 7 days (one week). On the "Patch change day", Day 8, remove the used patch. Apply a new patch immediately. The used patch still contains some medicine - throw it away by carefully folding it in half, so that it sticks to itself.
7) You will apply a new patch on week 2 (Day 8 ), and again on week 3 (Day 15), on your "Patch change day". To avoid irritation, do not apply the new patch to the exact same spot on your skin.
8 ) Do not wear a patch on week 4 (Day 22 through Day 28 ). You should have your period during this week.
9) Begin your next four-week cycle by applying a new patch on your normal "Patch change day", the day after Day 28 - no matter when your period begins or ends.
If your patch becomes loose or falls off:
- For less than 1 day: try to re-apply it, or apply a new patch immediately. No back-up contraception is needed. Your "Patch change day" will remain the same.
- For more than one day OR if you are not sure for how long: YOU MAY BECOME PREGNANT. Start a new 4-week cycle immediately by putting on a new patch. You now have a new Day 1 and a new "Patch change day". You must use back-up contraception for the first week of your new cycle.
- Do not try to re-apply a patch if it is no longer sticky, if it has become stuck to itself or another surface, if it has another material stuck to it, or if it has become loose or has fallen off before. No tapes or wraps should be used to keep the patch in place. If you cannot re-apply a patch, apply a new patch immediately.
If you forget to change your patch:
- At the start of any patch cycle: Week 1 (Day 1): YOU MAY BECOME PREGNANT -- you must use back-up contraception for one week. Apply the first patch of your new cycle as soon as you remember. You now have a new "Patch change day" and a new Day 1.
- In the middle of your patch cycle: Week 2 or Week 3: If you forget to change your patch for one or two days, apply a new patch as soon as you remember. Apply your next patch on your normal "Patch change day". No back-up contraception is needed.
--> Week 2 or Week 3: If you forget to change your patch for more than 2 days, YOU MAY BECOME PREGNANT -- start a new 4-week cycle as soon as you remember by putting on a new patch. You now have a different "Patch change day", and a new Day 1. You must use back-up contraception for the first week of your new cycle.
- At the end of your patch cycle:Week 4: If you forget to remove your patch, take it off as soon as you remember. Start your next cycle on your normal "Patch Change Day". No back-up contraception is needed.
- At the start of your next patch cycle: Day 1 (week 1): If you forget to apply your patch, YOU MAY BECOME PREGNANT - apply a new patch as sson as you remember. You now have a new "Patch Change Day" and new Day 1. You must use back-up contraception for the first week of your new cycle.
- You should never have the patch off for more than 7 days.
Other Information
- Always apply your patch to clean, dry skin. Avoid skin that is red, irritated or cut. Do not use creams, oils, powders or make-up on your skin where you will put a patch, or near a patch you are wearing. It may cause the patch to become loose.
- If patch use results in uncomfortable irritation, a new patch may be applied to a new location until the next Change Day. Only one patch should be worn at a time.
- Some medicines may change the way the Transdermal System works. I you are taking any medication, you must talk to your healthcare provider BEFORE you use the patch. You may need to use back-up contraception.
- Store between 15 - 30 degrees Celsius (59 - 86 degrees Fahrenheit).
- Single replacement patches are available through your pharmacist.
Disposal of Evra
Throw away the used patch by carefully folding it in half so the adhesive side sticks to itself, and dispose it in the garbage out of reach of children and pets.
When You Switch From the Pill to Evra
If you are switching rom the pill to the contraceptive patch, wait until you get off your menstrual period. If you do not get your period within 5 days of taking your last active pill, check with your doctor or clinic before starting Evra.
Important Points to Remember
1) It is important to use the contraceptive patch exactly as described in this leaflet. Dosing errors increase your chances of becoming pregnant. This includes starting your contraceptive cycle late or missing your scheduled [Patch] Change Days.
2) You should wear one patch per week for three weeks, followed by one week off. You should never have the patch off for more than 7 days in a row. If you have the patch off for more than 7 days in a row, and you have sexual intercourse during this time, YOU MAY BE AT RISK OF PREGNANCY. Check with your doctor or clinic.
3) If you are not sure what to do about dosing errors:
- Use a back-up method anytime you have sex.
- Contact a healthcare provider for instructions.
4) Do not skip patches, even if you don't have sex very often.
5) Many women have spotting or light bleeding, breast tenderness or may feel sick to their stomach during the first 3 cycles. If these symptoms occur, do not stop using the contraceptive patch. The problem will usually go away. If it does not go away, check with your doctor or clinic.
6) Mistakes in using patches can also cause spotting or light bleeding.
7) If you miss 2 periods in a row, contact your doctor or clinic because you might be pregnant.
8 ) Unlike the Pill, the amount of drug you get from the Evra patch should not be affected by vomiting or diarrhea.
9) If you are taking additional medicines, including herbal medicines, drugs purchased without prescriptions, or any other drugs prescribed by your doctor, your contraceptive patch may not work as well. Use a non-hormonal back-up method (such as condoms, spermicidal foam or contraceptive sponge) until you check with your doctor or clinic.
10) If you want to move your Patch Change Day to a different day of the week, contact your doctor.
11) Be sure you have ready at all times:
- A non-hormonal birth control (such as condoms, spermicide or contraceptive sponge) to use as a back-up in case of dosing errors.
12) If you have trouble remembering to change your contraceptive patch, talk to your doctor or clinic about how to make patch-changing easier, or about using another method of birth control.
13) Single replacement patches are available through your pharmacist.
14) For patch replacement, see the "How to Use Evra" section. [Scroll up]
If you have any questions or unsure about the information in this leaflet, call your doctor or clinic.
Missed Periods
There may be times when you may not menstruate regularly during your patch-free week. If you have used your contraceptive patches correctly and miss one menstrual period, continue using your contraceptive patch for the next cycle but be sure to inform your healthcare provider before doing so.
If you have not used your contraceptive patches as instructed and missed a menstrual period, or if you have missed two consecutive menstrual periods, you may be pregnant. Check with your healthcare provider immediately to determine whether you are pregnant. Stop using the contraceptive patch and use a non-hormonal method of birth control until you are sure you're not pregnant.
Pregnancy Due to Contraceptive Patch Failure
The incidence of pregnancy from hormonal contraceptive failure is approximately 1% (ie - 1 pregnancy per 100 women per year) if used correctly. The chance of becoming pregnant increases with incorrect use. If contraceptive patch failure does occur, the risk to the fetus is minimal.
Pregnancy After Stopping Evra
There may be some delay in becoming pregnant after you stop using the contraceptive patch, especially if you had irregular menstrual cycles before you used the contraceptive patch. It may be advisable to postpone conception until you begin menstruating regularly once you have stopped using the contraceptive patch and desire pregnancy.
There does not appear to be any increase in birth defects in newborn babies when pregnancy occurs soon after stopping the contraceptive patch.
|
 |
 |
|
|
|
|
|
|
|
|
|
|
|
|
 Posted: Sun Jun 28, 2009 9:31 pm Posted: Sun Jun 28, 2009 9:31 pm
The Ortho Evra Patch - Additional and Supplementary Information(From the old Evra Patch Info Sticky) Supplementary Information For Patients Considering the Use of EvraRead this information carefully and discuss it with your doctor. IntroductionThe following information will help you to make an informed choice on the use of the Evra contraceptive patch. You should read this information if you are thinking about any method of birth control. If you have decided to use Evra, this information will help you understand both the risks and the benefits. This information will also give you detailed instructions on how to use the Evra transdermal system. When Evra is used as directed, it is a very effective way to prevent pregnancy; the chance of becoming pregnant is comparable to that of combination birth control pills. Evra is convenient and has many benefits other than birth control. Most women do not develop serious and unpleasant side effects from using hormonal contraceptives, including Evra. Evra has important advantages over other methods of birth control. It also has certain risks that other methods do not have. Your doctor is the best person to explain the consequences of any possible risks. You can help your doctor prescribe Evra as safely as possible. Tell your doctor about yourself, and be alert for the earliest signs of possible trouble. Do not use the drug for any condition other than the one for which it was prescribed. This drug has been prescribed specifically for you; do not give it to others who want birth control. The Evra transdermal system is a "combination" hormonal contraceptive. It contains two female sex hormones - an estrogen and a progestin. The amount of estrogen is more important. The effectiveness and some dangers of hormonal contraceptives are related mainly to the amount of estrogen. How the Contraceptive Patch WorksThe contraceptive patch works in two ways: 1) It inhibits a monthly release of an egg by the ovaries. 2) It changes the mucus produced by the cervix. This slows the movement of the sperm throuh the mucus and through the uterus (womb). Effectiveness of Hormonal Contraceptive MethodsWhen Evra is used correctly, the chance of becoming pregnant is comparable to that of combination birth control pills which are more than 99% effective in preventing pregnancy (when: the pills are TAKEN AS DIRECTED, and the amount of estrogen is 20 pg [?] or more). A 99% effectiveness rate would mean that if 100 women used the contraceptive patch for one year, one woman in the group would become pregnant. The change of becoming pregnant increases with incorrect use. Other Ways to Prevent PregnancyOther methods of birth control are available to you. They are usually less effective than hormonal contraceptive methods such as the birth control pll or Evra. When used properly, however, other methods of birth control are effective enough for many women. The following table [in the next section] gives reported pregnancy ratesfor various forms of birth control, including no birth control. The reported rates represent the number of women out of 100 who would become pregnant in one year. Reported Pregnancies Per 100 Women Per YearCombination Pill = less than 1 - 2 Intrauterine Device (IUD) = less than 1 - 6 Condom with spermicidal foam or gel = 1 - 6 Mini-pill = 3 - 6 Condom = 2 - 12 Diaphram with spermicidal foam or gel = 3 - 18 Spermicide = 3 - 21 Sponge with spermicide = 3 - 28 Cervical cap with spermicide = 5 - 18 Periodic abstinence (rhythm method), all types = 2 - 20 No birth control = 60 - 85 Pregnancy rates vary widely because people differ in how carefully and regularly they use each method. (This does not apply to IUD's since they are implanted in the uterus.) Regular users may achieve pregnancy rates in the lower ranges. Other many expect pregnancy rates more in the middle ranges. The effective use of birth control methods other than the contraceptive pathc may require more effort than replacing a single patch every week for three out of four weeks. It is an effort that many couples undertake successfully. Who Should Not Use Hormonal ContraceptionYou should not use the Evra contraceptive patch if you have or have had any of the following conditions: - Unusual vaginal bleeding that has not yet been diagnosed. - Blood clots in the legs, lungs, eyes or elsewhere. - A stroke, heart attack, or chest pain (angina pectoris). - Known or suspected cancer of the breast or sex organs. - Liver tumor associated with the use of the Pill or other estrogen-containing products. - Jaundice or liver disease if still present, and/or - Yellowing of the whites of your eyes, or of the skin (jaundice) during pregnancy or during use of hormonal contraceptives such as Norplant [the implant] or the birth control pill. Evra should not be used if you are pregnant or if pregnancy is suspected. Be sure to inform your doctor or healthcare provider if you weigh more than 198 lbs, are currently breastfeeding, or are on any medications. There are also conditions that your doctor will want to watch closely, or that might cause your doctor to recommend a method of contraception other than the contraceptive patch: - Breast conditions - a strong family history of breast cancer, breast disorders including pain, discharge from the nipples, thickenings, or lumps. In some cases, benefit may be derived from using the contraceptive patch; In other cases, adverse effects may follow. - Diabetes. - High blood pressure. - Abnormal levels of fats in the bloodstream (high cholesterol or trigylcerides). - Cigarette smoking. - Migraine headaches. - Heart or kidney disease. - Epilepsy. - Depression. - Fibroid tumors of the uterus. - Gallbladder or pncreatic disease. - Plans for forthcoming surgery. - History of jaundice or other liver disease. You should also inform your doctor about a family history of blood clots, heart attacks or strokes. The Risks of Hormonal Contraception1) Circulatory disorders (including blood clots in legs, lungs, heart, eyes, or brain).Blood clots are the most common serious side effects of hormonal contraceptives, including the contraceptive patch. Clots can occur in many area of the body: - In the brain, a blood clot can result in a stroke. - In a blood vessel in the heart, a clot can result in a heart attack. - In the legs and pelvis, a clot can break off and travel to the lungs, resulting in a pulmonary embolus. - In a blood vessel leading to an arm or leg, a clot can result in damage or the loss of a limb. Any of these conditions can cause death or disability. Clots also occur rarely in the blood vessels of the eye, resulting in blindness or impaired vision. Women who use hormonal contraceptives have a higher incidence of blood clots. The risk of clotting seems to increase with higher estrogen doses. It is important, therefore, to use as low a dose of estrogen as possible. Evra delivers an average dose og 20pg [?]/day of the estrogen, ethinyl estradiol. Cigarette smoking increases the risk of serious adverse effects on the heart and blood vessels. This risk increases with age and becomes significant in hormonal contraceptive users over 35 years of age. Women should not smoke.2) Breast cancer. The most significant risk factors for breast cancer are increasing age and a strong history of breast cancer in the family (mother or sister). Other established risk factors include obesity, never having children, and having your first full-term pregnancy at a late age. Some women who use hormonal contraceptives may be at an increased risk of developing breast cancer before menopause which occurs around age 50. These women may be long-term of hormonal contraceptives (more than 8 years) or women who start using hormonal contraceptives at an early age. In a few women, the use of hormonal contraceptives may accelerate the growth of an already existing but undiagnosed breast cancer. Early diagnosis, however, can reduce the effect of breast cancer on a woman's life expectancy. The potential risks related to hormonal contraceptives seem to be small, however. Some studies have found an increase in the incidence of cancer of the cervix in women who use oral contraceptives, although this finding may be related to factors other than the use of oral contraceptives. However, there is suficient evidence to rule out the possibility that oral contraceptives may cause such cancers. Women with the following conditions should be examined by their doctors yearly no matter what method of contraception they use: - A strong history of breast cancer in the family. - Breast nodules or thickenings. - Discharge from the n****e. 3) Damages to developing child if hormonal contraceptives are used during pregnancy.Hormonal contraceptives, including the Evra contraceptive patch, should not be taken by a pregnant woman. There is no evidence, however, that hormonal contraceptives can damage a developing child. Further, there is no evidence that the use of hormonal contraceptives immediately before a pregnancy will adversely affect a baby's development. When a woman stops taking the contraceptive patch to become pregnant, however, her doctor may recommend a different method of contraception until she has a period on her own. In this way, the pregnancy can be more accurately dated. You should check with your doctor about risks to your unborn child from any medication taken during pregnancy. 4) Gallbladder disease and liver tumors.Users of hormonal contraceptives, including the contraceptive patch, have a greater risk of developing gallbladder disease requiring surgery within the first year of use. The risk may double after four or five years of use. The short and long-term use of birth control pills have been linked with the growth of liver tumors. Such tumors are EXTREMELY rare. Since the contraceptive patch contains hormones similar to those in birth control pills, this association may exist with the contraceptive patch. 5) Skin irritation.Skin irritation, redness or rash may occur at the site of application. If this occurs, a new patch may be applied to a new location until the next Patch Change Day. 6) Other side effects of Evra.Some users of hormonal contraceptives, including the Evra contraceptive patch, have unpleasant side effects. These side effects are temporary and not hazardous to health. There may be tenderness of the breasts, nausea, and vomiting. Some users will experience weight gain or loss. Many of these side effects have occured with high-dose combination birth control pills. These side effects are less common with the loss-dose pills prescribed today and are expected to be less common with the contraceptive patch. Unexpected vaginal bleeding or spotting, and changes in the usual menstrual period also may occur. These side effects usually disappear after the first few cycles of contraceptive patch use, but may also occur after you have been using the contraceptive patch for some time. They are NOT an indication to stop using the contraceptive patch. If the bleeding occurs in more than one cycle, or lasts for more than a few days, talk to your doctor or healthcare provider. Unless more significant complications occur, a decision to stop using the patch or to change to the use of another hormonal contraceptive should be made only after three consecutive months of use. Occasionally, users develop high blood pressure that may require stopping the use of the contraceptive patch. Other side effects may include: - Growth of pre-existing fibroid tumors of the uterus. - Depression. - Liver problems with jaundice (yellowing of the skin). - An increase or decrease in hair growth, sex drive and appetite. - Skin pigmentation. - Headaches. - Rash and/or - Vaginal infections. Infrequently, there is a need to change contact lens prescription or an inability to use contact lenses. A woman's menstrual period may be delayed after stopping the use of the contraceptive patch. There is no evidence that the use of the contraceptive patch leads to a decrease in fertility. As mentioned, it is wise to delay starting a pregnancy for one menstrual period after stopping the use of the contraceptive patch. Non-Contraceptive Benefits of Hormonal ContraceptivesSeveral health advantages have been linked to the use of hormonal contraceptives: - Reduction in the incidence of cancer of the uterus and ovaries. - Reduction in the likelihood of developing benign (non-cancerous) breast disease and ovarian cysts. - Less menstrual blood loss and more regular cycles. The risk of developing iron-deficiency anemia is this reduced. - There may be a decrease in painful menstruation and premenstrual syndrome (PMS). - Acne, excessive hair growth and male hormone-related disorders also may be improved. - Ectopic (tubal) pregnancy may occur less frequently. - Acute pelvic inflammatory disease may occur less frequently. The Evra contraceptive patch (like all hormonal contraceptives) DOES NOT PROTECT against sexually transmitted diseases (STD's), including HIV/AIDS, chlamydia, genital herpes, genital warts, gonorrhea, hepatitis B, and syphilis. For protection against STD's, it is advisable to use latex condoms IN COMBINATION WITH the contraceptive patch.Periodic ExaminationA complete medical and family history is necessary before the Evra contraceptive patch is prescribed. A physical exam should include measuring blood pressure, and examining the breasts, abdomen, pelvic organs, and limbs. A second visit to your doctor should take place 3 months or sooner after starting Evra. During this visit, any side effects should be evaluated and yoru blood pressure checked again. Afterwards, an annual examination similar to the visit is recommended. A Pap smear is usually taken before starting hormonal contraceptives, and then at intervals recommended by your doctor. ------------------ (From the old Evra Patch Info Sticky) Additional Ortho Evra InformationTaken from: http://www.hc-sc.gc.ca/dhp-mps/medeff/advisories-avis/public/2006/evra_pc-cp_e.html November 21, 2006 Subject: New safety information about EVRA* (norelgestromin and ethinyl estradiol) Transdermal System Janssen-Ortho Inc., in consultation with Health Canada, wishes to highlight important new safety information pertaining to EVRA*. The EVRA* transdermal system marketed in Canada contains 6.0 mg norelgestromin (NGMN) and 0.60 mg ethinyl estradiol (EE) and is approved for use in contraception (prevention of pregnancy). ORTHO EVRA® is the formulation of EVRA* marketed in the United States and contains 6.0 mg NGMN and 0.75mg EE. Although EVRA* and ORTHO EVRA® are manufactured differently and therefore contain different total amounts of estrogen, the risk of side effects reported for ORTHO EVRA® is considered to apply equally to the EVRA* formulation available in Canada. - The results of a recent study indicate that women using the ORTHO EVRA contraceptive patch (the formulation of EVRA marketed in the United States) had an increased risk of blood clots in the legs and lungs compared to women using an oral contraceptive. Another study indicated no difference in the risk of blood clots in the legs and lungs in women using ORTHO EVRA compared to women using an oral contraceptive. - Women who are obese are at particularly high risk of blood clots. - Due to a theoretical risk of unintentional increase in estrogen exposure from the patch, patients are recommended not to expose the patch area to sources of heat such as sauna or whirlpool bath. - A recent study showed that the EVRA transdermal system sold in Canada produced a similar total estrogen exposure in patients compared to taking a typical birth control pill. The current Canadian labeling information on EVRA contains a description of the risks and proper use of the product. There is also a detailed section on the importance of discontinuing the medication at the earliest sign of blood clots. Common symptoms of blood clots can include, but are not limited to, pain the calf, shortness of breath, chest pain or coughing blood. Patients concerned about the risks and benefits of EVRA should speak to their physician. Janssen-Ortho Inc. has provided this information to physicians, nurses and pharmacists across Canada. This advisory and letters issued to physicians, nurses and pharmacists can be accessed at Health Canada's website at: http://www.hc-sc.gc.ca/dhp-mps/medeff/advisories-avis/index_e.html This information is also available at http://www.janssen-ortho.com. For more information, patients should consult their health care professional. Patients should NOT discontinue their medication without consulting their physician or pharmacist first. If you have questions about EVRA, please talk to your doctor or take the medication back to your pharmacy and speak to your pharmacist. For further information on Janssen-Ortho Inc.: call Suzanne Frost, Janssen-Ortho Inc., (416) 449-9444 or call the Janssen-Ortho Medical Information Department at 1-800-567-3331, from 9 a.m. to 5 p.m. Monday to Friday, EST. The identification, characterization, and management of marketed health product-related adverse reactions are dependent on the active participation of health care professionals in adverse drug reaction reporting programmes. Any occurrences of serious and/or unexpected adverse reactions in patients receiving EVRA, including cases of fatality or blood clots, should be reported to Janssen-Ortho Inc. or the Marketed Health Products Directorate at the following addresses: Janssen-Ortho Inc. 19 Green Belt Drive Toronto, Ontario M3C 1L9 Or call toll-free at 1-800-567-3331 Or email to dsscan@joica.jnj.com Or toll-free fax to 1-866-767-5865 Any suspected adverse reaction can also be reported to: Canadian Adverse Drug Reaction Monitoring Program (CADRMP) Marketed Health Products Directorate HEALTH CANADA Address Locator: 0701C OTTAWA, Ontario, K1A 0K9 Tel: (613) 957-0337 or Fax: (613) 957-0335 To report an Adverse Reaction, consumers and health professionals may call toll free: Tel: 866 234-2345 Fax: 866 678-6789 cadrmp@hc-sc.gc.ca The AR Reporting Form and the AR Guidelines can be found on the Health Canada web site or in The Canadian Compendium of Pharmaceuticals and Specialties. For other inquiries related to this communication, please contact Health Canada at : Bureau of Metabolism, Oncology and Reproductive Sciences (BMORS) E-mail: bmors_enquiries@hc-sc.gc.ca Tel: (613) 941-3171 Fax: (613) 941-1365 If you want more information about birth control patches, ask your doctor or pharmacist. Keep out of reach of children.
|
 |
 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
 Posted: Sun Jun 28, 2009 9:45 pm Posted: Sun Jun 28, 2009 9:45 pm
Nuva Ring(From the old birth control sticky) Taken from: http://www.mypleasure.com/education/contraception/nuvaring.asp Birth Control Method Type: Hormonal DescriptionThe Ring is marketed under the brand name NuvaRing. It is a soft, flexible ring (about two inches in diameter) that is inserted into the v****a once a month. It stays in place for three weeks, and is removed for the fourth week. You should have your period during the fourth week. How It WorksThe muscles in the vaginal wall keep NuvaRing in place. While in the v****a, it slowly releases low doses of the hormones progestin and estrogen. This prevents the ovaries from releasing an egg (ovulation). Should You Use It?The Ring is great for women who want an easy-to-use method of birth control. There is nothing to remember on a daily or weekly basis. EffectivenessNuvaRing has been proven to be 99% effective, the same as the Pill, when used as directed. STI ProtectionThe Ring does not prevent the transmission of sexually transmitted infections (STIs), including HIV. Advantages - The Ring is easy to use; it is inserted and removed just once a month. - This method uses less than half of the estrogen used in some birth control pills. - You don't have to remember a pill each day, as with oral contraceptives. - Since the Ring releases a steady, consistent dose of hormones each month, it produces a lower incidence of headaches, nausea, breakthrough bleeding and breast tenderness then most oral contraceptives. - The Ring causes fewer hormonal ups and downs than most hormonal methods. - Doesn't require any interruption of sex play to protect against pregnancy. Disadvantages - Normally, the Ring stays in place. If it should fall out, follow the manufacturer's instructions for reinsertion. If it is out for longer than 3 hours, you will need to reinsert the Ring, and then use another form of birth control for the next 7 days. - NuvaRing requires a prescription. - Some women experience increased vaginal discharge or vaginal infection. - The risk of getting blood clots may be greater with the type of progestin in NuvaRing ? than with some other progestins in certain low-dose birth control pills. - It is unknown if the risk of blood clots is different with NuvaRing ? use than with the use of certain birth control pills. - Cigarette smoking increases the risk of high blood pressure and heart disease; women who use combination hormonal contraceptives are strongly advised not to smoke. - NuvaRing ? does not protect you from HIV or other infections. - Consult with your health care provider to determine whether you have any medical conditions that would be intensified while using NuvaRing ? . Where to Buy ItIn the United States, The Ring requires a prescription. You can get NuvaRing ? from your doctor, nurse practitioner, nurse midwife, health department or family planning clinic. Follow UpConsult your doctor for complete information on potential side effects. ----------------- Additional NuvaRing information: http://www.nuvaring.com/Consumer/index.asp?SetSession=Yes&strGUID={16C99EAC-6975-4820-9D56-F590633384E5}&SID=145832701 (link provided by Perri Indiya! heart ) ----------------- More NuvaRing information: From the official Nuva Ring website: - What is Nuva Ring?- Is Nuva Ring for me?------------------- Taken from: http://www.mckinley.uiuc.edu/Handouts/nuvaring/nuvaring.htmNuvaRing is a soft flexible ring that is approximately two inches in diameter. The ring is worn in the v****a for three weeks. It is then removed for one week. The menstrual period will usually occur during this week. NuvaRing contains a combination of estrogen and progestin hormones similar to the hormones used in most birth control pills and in the patch. The primary difference is in the method by which the medication is delivered into the body. The hormones contained within the ring are absorbed continuously, directly into the blood stream through the vaginal wall. HOW DOES THE RING WORK?The estrogen and progestin hormones are similar to the natural hormones produced by the ovaries. The progestin component is absorbed in small amounts and prevents the ovary from releasing an egg (ovulation). The uterine lining also becomes thinner than usual, which would inhibit implantation of a fertilized egg. In addition, the cervical mucus also becomes thicker and this helps prevent sperm from entering the uterus. When properly placed, the ring is held in place by the vaginal muscle structure, even during exercise or intercourse. The NuvaRing� cannot �get lost� in the v****a. The v****a is flexible, but no longer than the palm of your hand. The cervix forms the back wall of the v****a so the ring remains in the v****a. HOW EFFECTIVE IS NuvaRing?According to studies provided to the Food and Drug Administration (FDA) during the approval process, effectiveness ratings are listed at 99% when used according to label instructions. This is comparable to the patch and better than the Pill's effectiveness ratings. WHAT ARE THE BENEFITS OF USING NuvaRing?- Medication is absorbed directly into the blood stream through the vaginal wall membrane providing a consistent level of medication in the blood, which improves effectiveness and helps limit side effects. Oral contraceptives take time to be absorbed into the blood stream and this causes peaks and valleys in the hormone blood levels. - Once monthly insertion eliminates the need to think about birth control on a daily or weekly basis; usually neither partner is aware of its presence during intercourse. - Very discreet and private; no one can see it or know that you are wearing it. - Easily reversible - ovulation returns quickly when use of the ring is discontinued; however, women who have irregular menstrual cycles will probably return to the irregular cycle. - Provides a regular menstrual period, but menses are usually lighter and may be shorter than a normal period. - Thickened cervical mucus helps decrease the risk of pelvic inflammatory infections. - Reduces the chances of ovarian cysts and tubal pregnancy. - Vomiting and diarrhea should not interfere with the effectiveness of the ring. ARE THERE OTHER THINGS THAT SHOULD BE CONSIDERED?- Insertion and removal require that a woman insert her finger inside the v****a; therefore she must be comfortable touching her genitalia and v****a. - NuvaRing does not offer any protection against transmission of sexually transmitted infections (STIs), such as chlamydia, gonorrhea, syphilis, hepatitis or HIV. Condoms may be used with the ring to reduce the risk of STIs. - Always inform your health care provider that you are using the ring. It is a medication just like any others that you are taking. - Disposal is easy - Keep the original foil package and when the ring is removed just place it back in the foil pack, seal and throw away. - NuvaRing is nonabsorbent, odorless, and contains no latex. - Do not breast feed while using NuvaRing.- If for any reason, the ring is removed or slips out, it may be rinsed in cool water and reinserted. If it is out for three hours or more, there will be reduced contraceptive protection and an alternative method of birth control must be used until the ring has been in place for seven consecutive days. Emergency contraception is available if it is out three hours or longer. - Unopened NuvaRing packs will expire in four months unless stored in the refrigerator. (Refer to the package insert for additional information or talk with the pharmacist.) - If unopened NuvaRing packs are stored in temperatures greater than 86 degrees Farenheit, the effectiveness may be lessened. - It is safe to use other vaginal medications/lubricants with the NuvaRing. WHAT ABOUT CANCER AND THE NuvaRing?There is little information available specifically about the ring and cancer. However, since the ring and birth control pills utilize the same types of hormones, it is expected to have similar effects. That information is included for your review. Since 1960, when birth control pills first became available, important information has been learned about pills and cancer. Pills reduce the risk of ovarian cancer � three years of use reduces the risk of ovarian cancer by 40%; ten years reduces the risk by 80%. Pills reduce the risk for endometrial (uterine lining) cancer. Most studies suggest that pills neither reduce nor increase the risk for breast cancer. Research continues to evaluate this. Women are encouraged to do monthly self-breast exams and report any changes or problems to their health care provider. Some studies indicate an increased incidence of cervical cancer. However, this may be more related to factors such as numbers of sexual partners, STI exposure, etc., than to birth control pill use. Annual pap smears provide the best screening for cervical cancer. WHAT ABOUT DRUG INTERACTIONS?Contraceptive effectiveness may be reduced when hormonal contraceptives are administered at the same time other drugs are being taken. Break through bleeding or unintended pregnancy can result. Examples of drugs that potentially interfere with contraceptive hormones include antifungals, seizure medications and, potentially, antibiotics. For additional information please refer to the handout Pill Interactions with Other Drugs. ARE THERE RISKS ASSOCIATED WITH USE OF NuvaRing?Health risks related to the contraceptive ring are low when compared to the risks of pregnancy and childbirth and are the same as with the birth control pill and the patch. The risks are usually associated with the estrogen component in the ring. In a small number of women estrogen affects the way the body forms blood clots. This may cause blood clots to form in the legs, lungs, brain or other vital organs causing serious health problems. Cigarette smoking increases the risk of cardiovascular complications and is greater when a woman smokes more than 15 cigarettes daily and increases significantly when a she is also over 35 years of age. Women are advised to quit smoking if they use hormonal contraception in any form. Other factors increasing the risk of blood clots are high cholesterol, diabetes, high blood pressure, obesity, and migraine headaches with aura or neurological symptoms. If you experience any of the following symptoms, you should seek medical care immediately. A - Abdominal pain (severe) C - Chest pain, shortness of breath, coughing up blood H - Headache (severe), numbness or weakness in arms or legs E - Eye problems (vision loss, blurring, flashing lights) S - Severe leg pain in calf or thigh WHAT ARE THE SIDE EFFECTS?The estrogen component is responsible for many of the side effects that occur with all of the combined hormonal methods of birth control (ring, patch or pill). The ring has less estrogen than either the pill or the patch; therefore nausea, headaches and breast tenderness may occur less often or be less severe. The most common side effect is an increased amount of normal vaginal discharge. Occasionally women report an increased number of vaginal infections and irritation. Clinical studies show women using the ring experience an increased amount of lactobacillus in the v****a. Lactobacillus is a normal bacteria present in the v****a that actually helps decrease the incidence of yeast infections. Headaches may occur. These should be reported to your health care provider right away if the headache or accompanying symptoms (light sensitivity, nausea, vomiting, etc.) is more severe than you have experienced before, do not respond to over-the-counter medications or last more than one month. Mild nausea may occur with initial use, but usually will resolve within a few days. Rarely, vomiting may occur. If nausea lasts throughout the month or occurs persistently at the beginning of every ring cycle, report it to your health care provider. Vitamin B-6 (50 mg. 1-2 tablets daily) may help reduce nausea. Weight gain may occur, but is usually limited to a few pounds. Moodiness may occur within the first 1-2 months of use, but will usually diminish with continued use. Vitamin B-6 (50 mg. 1-2 tablets daily) may help decrease moodiness as well as relieve nausea. Notify your provider right away if severe depression symptoms occur. Occasionally spotting and mid-cycle bleeding may occur while the ring is in the v****a. The amount of bleeding is usually minimal and will normally be reduced as you continue use, but may occur from time to time for no apparent reason. This is a normal occurrence and does not indicate that it is not working as a contraceptive. Reactions to any method of birth control will vary from person to person. For some the reaction will be beneficial, but others may find them detrimental. For instance, acne may improve for some, but worsen for others; cramps usually improve, but occasionally a woman will experience increased cramps instead. HOW DO I OBTAIN A NuvaRing PRESCRIPTION?A prescription for the ring can be obtained from a McKinley Women's Health provider or your health care provider at home. For a prescription from a McKinley provider, an annual exam within the past 12 months needs to be documented in the McKinley chart. First time users of hormonal birth control methods must complete the on-line birth control class at: http://www.mckinley.uiuc.edu/bcclass/classoptions1.html.If you are obtaining your prescription from your home provider, refer to the handout, Transferring Outside Contraceptive Prescriptions to McKinley, for additional information and instructions. WHEN DO I START USING NuvaRing?- If you are starting NuvaRing and HAVE NOT been using any other hormonal method of birth control (i.e. birth control pills or the patch): insert the ring between day one and five of your menses, even if you have not finished bleeding. Count the first day of your period as day one. You should use a condom during each act of intercourse for the first seven days during the first ring cycle. - If you are switching from birth control pills to the NuvaRing�: Insert the ring at any time during the seven days immediately following your last active birth control pill. It may be easiest to insert the ring on the day that you would have normally started a new pill pack. There should never be more than seven days between the last active pill and insertion of the ring. The ring may be inserted even if there is still some bleeding. No back up birth control is needed. - If you are switching from the patch to NuvaRing: Insert the ring at any time during the seven days immediately following the removal of Patch #3. There should be no more than seven days between removing the patch and inserting the ring. The ring may be inserted even if there is still some bleeding. No back up birth control is needed. - If you are switching from a progestin-only pill: Insert the NuvaRing on any day of the month. Do not skip any days between your last pill and the first day of NuvaRing use. Use a back-up method of birth control (condoms) for seven days. - If switching from DepoProvera to NuvaRing: Insert NuvaRing on the day your next injection is due. (12 weeks from previous injection plus or minus a week) Use a back up method of birth control (condoms) for seven days. - If starting NuvaRing after a first trimester abortion: Insert NuvaRing within the first five days after the abortion. No back up birth control is needed. If not started within the first five days, wait until the next menstrual period starts and insert within the first five days of bleeding. During the first cycle, use a back up method of birth control for seven days. WHEN DO I REMOVE THE NuvaRing?Remove the ring three weeks after insertion, at approximately the same time of day, if possible. Place it in the foil envelope in which it was originally packaged and throw away. Contraceptive protection continues throughout the ring-free week. WHEN DO I INSERT A NEW RING?Seven days after removing the old ring, insert a new one. It is recommended that you insert and remove it at the same time of day each month. For example if you insert the first ring at 7 a.m. Sunday morning, it should be removed at approximately 7a.m. Sunday three weeks later and reinserted on the following Sunday at approximately the same time. The ring may be inserted sooner than this time if it is more convenient. It should not be inserted later than seven days. You should expect your period during the ring-free week. Occasionally, due to the low dose of hormones used in the ring, you may experience a "missed" period (the absence of bleeding during the ring-free week). If this occurs, and the ring has been used properly, following all instructions, re-insert the ring as scheduled. For reassurance you may do a pregnancy test if you wish. If you miss two periods in a row, you should talk with your health care provider. If the ring has been out of the v****a for more than three consecutive hours, or was not inserted as scheduled, and unplanned intercourse (UPI) has occurred, you may wish to consider using Plan B. If the ring has been out of the v****a for more than three consecutive hours, or was not inserted as scheduled, and vaginal intercourse occurred without using a condom; you may want to consider using emergency contraception/Plan B. HOW DO I INSERT AND REMOVE THE NuvaRing?The NuvaRing may be inserted while standing, squatting or lying down. Using your thumb and index finger, press the sides of the ring together. Holding NuvaRing and pressing the sides together, gently push it deep into the v****a. The exact position is not important. You should not be able to feel the ring when it is properly placed. To remove the ring, reach into the v****a using your index finger. Hook the tip of your finger around the ring and pull gently. The ring will naturally fold slightly as it is removed from the v****a. WHAT IF I FORGET TO REMOVE THE RING ON TIME?If NuvaRing remains in the v****a for 1-7 extra days, remove it and re-insert a new ring after a one-week break. You will still have contraceptive protection during the extra week and during your period. Do not leave the ring out more than seven consecutive days. If it remains in place longer than four weeks, you may not have adequate protection against pregnancy. Remove the ring, take a one-week break and reinsert. Use a condom for back-up birth control until one week after the ring is re-inserted. If you do not have a menstrual cycle in three weeks, when you remove the re-inserted NuvaRing� you should do a home pregnancy test. For McKinley eligible students, home pregnancy test kits are available in the Resource Center at McKinley and the Illini Union. WHAT IF THE RING SLIPS OUT?If the ring is not inserted deep into the v****a it may slip out when straining to have a bowel movement or removing a tampon. If this occurs, rinse it with cool water and reinsert it as soon as possible. If it is out for less than three hours, there is no loss of contraceptive protection. If the ring is lost, reinsert a new ring and use it following the original insertion/removal schedule. If the ring is out of place for more than three hours, you must use condoms as a back up birth control method for seven days. You may also wish to consider using Plan B Emergency Contraception. If you are having problems with the ring slipping out of place frequently, talk with your health care provider. IS IT SAFE TO USE VAGINAL MEDICATIONS OR LUBRICANTS WHEN THE RING IS IN PLACE?Yes, you may use vaginal medications or water-based lubricants while the NuvaRing� is in place in the v****a. There will be no decrease in the contraceptive benefit. NuvaRing is a medication and you should always advise all health care providers that you are using NuvaRing for contraception.
|
 |
 |
|
|
|
|
|
|
|
|
|
|
|
|
 Posted: Sun Jun 28, 2009 9:52 pm Posted: Sun Jun 28, 2009 9:52 pm
IUD (Updated 1/13/2010 - see bottom of this post) (From the old birth control sticky) The IUD- must be obtained by prescription and inserted by clinician. - contains copper or hormones that: prevent sperm from joining with the egg (copper), (and/or) prevent fertilized egg from implanting in uterus. Effectiveness: 97.4% - 99.2% - not effective against STI's. Advantages: - nothing to put in place before intercourse. - cooper IUD's may be left in place for up to 5 years. - no daily pill. - no effect on hormone levels in the body. - IUD's with hormones may reduce menstrual cramps. Possible Problems: - temporary increase in cramps. - heavier and longer periods. - more than one sexual partner can increase chance of tubal infection, which may lead to sterility. - rarely, IUD can move out of the uterus, into the abdomen or into the v****a. ---------------------- Taken from: http://www.womenshealthmatters.ca/centres/sex/birthcontrol/mirena.htmlMirena IUD (inter-uterine device)Mirena is a unique type of IUD that contains low doses of progestin: the same hormone used in some birth control pills. Like other IUDs, the Mirena is a small T-shaped device placed into the uterus by your health care provider. Because the hormones are released directly into the uterus, only low doses are necessary to prevent pregnancy, about 1/7 of that in a birth control pill. Mirena is about 99 percent effective in preventing pregnancy, similar to the birth control pill. This is significantly higher than a conventional copper IUD, which is 96-98 percent effective. Mirena does not protect you and your partner against sexually transmitted infections. Copper IUDs are not recommended for women with heavy menstrual periods, because they often make the bleeding heavier. However Mirena will reduce a woman's periods, and may be a useful treatment for women with small to moderate fibroids or heavy menstrual bleeding. Using MirenaMirena must be inserted in a doctor's office or clinic. It is often inserted during your period or shortly after having an abortion or giving birth when your caregiver can be sure that you are not pregnant. The insertion takes about five minutes. It is inserted into the uterus so that thin strings attached to the base of the T hang down through the cervical opening. These strings are trimmed so they are just long enough for you to check that the IUD is in place and so that a health care provider can use them to remove the IUD at a later date. Most women have some cramps when the IUD is being inserted. You may want to use another method of birth control as back-up for a month in case the IUD moves or comes out. After six weeks, return to your doctor or clinic for a check-up then continue to have your regular check-ups. The Mirena can remain in place for 5 years and can be easily and quickly removed by a health care provider. Changes to your Menstrual Cycle and other Side EffectsMirena will change your menstrual cycle and eventually make your periods much lighter. However, in the first three months of use, many women experience unpredictable bleeding, and about 20 percent have prolonged periods that last more than 8 days. After three months bleeding becomes more regular and may stop altogether. In studies of Mirena, women's periods were reduced by 85 percent after three months and 97 percent after a year. Although bleeding is much lighter, some women who use Mirena have difficulty predicting when their period will occur. Beyond these menstrual irregularities, Mirena has few side effects because it contains such a small amount of hormone. Some women do experience mild side effects related to the hormones such as headaches, water retention, breast tenderness or acne. Often these resolve after the first two months of use. Advantages- very effective - neither partner can feel an IUD during sex - the woman controls this method of birth control - can remain in place for many years Disadvantages- cost - does not protect against sexually transmitted infections - unpredictable bleeding and other side effects particularly in the first few months - increased risk of pelvic infection mainly associated with insertion - increased risk of benign ovarian cysts - may be difficult to insert in some women - rarely an IUD may puncture the wall of the uterus --------------------- More IUD Information:- Wikipedia: http://en.wikipedia.org/wiki/Intrauterine_device- http://www.birth-control-comparison.info/iudinfo.htm--------------------- Mirena Information [pamphlet] Information on MirenaThe following information is provided to answer the most commonly asked questions about Mirena (levonorgestrel-releasing intrauterine system). Please read it carefully before making a decision to use the product. The information provided applies only to Mirena. If you have any questions or you are not sure about something, please ask your doctor. What is Mirena?Mirena is an intrauterine system which prevents pregnancy by slowly releasing small amounts of a synthetic sex hormone known as levonorgestrel into the uterus. Levonorgestrel is a hormone commonly used in combination with oral contraceptives (the “Pill”) and is similar to progesterone, a sex hormone produced naturally by the body. What Does Mirena Look Like?Note: These pictures are of Mirena in a woman's body. They are not "real world" pictures, just depictions, but if you're uncomfortable with the topic then please view the pictures at your own risk. Mirena: 1, 2, 3, and 4. Mirena consists of a small white T-shaped frame made from soft, flexible plastic. The vertical and horizontal arms of the T are approximately 3cm in length. The vertical arm is surrounded by a narrow cylindrical shaped reservoir that contains levonorgestrel. Two fine plastic threads are attached to the tip of the vertical arm. These threads are intended to be used for the removal of the system and also serve to check its presence once it is in place. How Does Mirena Work?Mirena works by slowly releasing levonorgestrel into the uterus at a rate of approximately 20 micrograms per day. This small amount of levonorgestrel prevents pregnancy by: - Reducing the normal monthly thickening of the lining of the uterus. - Thickening the cervical mucus which prevents passage of the sperm through the cervical canal (opening to the uterus). Mirena contains a total of 52mg of levonorgestrel which is enough hormone to prevent pregnancy for 5 years. How Effective is Mirena?For preventing pregnancy, Mirena is as effective as oral contraceptives. Clinical trials found that there were about 2 pregnancies every year for every 1,000 women using Mirena. Can Any Woman Use Mirena?Most women can use Mirena, but it is not suitable for everyone. Your doctor will examine you and ask about your medical history in order to decide whether or not you can use it. Tell your doctor if you: - Are sensitive to the hormone levonorgestrel. - Are pregnant or suspect that you are pregnant. - Are breast-feeding. - Have an unusual menstrual bleeding pattern. - Have an abnormal uterus or fibroids. - Have an unusual or unpleasant vaginal discharge or vaginal itching. - Have or have had pelvic inflammatory disease. - Have had a stroke, heart attack or any heart problems. - Have or have had liver problems. - Have immunodeficiency (a doctor will have told you if you have this). - Have or have had cancer, suspected cancer or leukemia. - Have or have had trophoblastic disease (a doctor will have told you if you have this). - Are diabetic, have high blood pressure or abnormal blood lipid levels. - Have a history of blood clots (thrombosis). - Are on long-term steroid therapy or are taking any other medications. - Have or develop migraine, dizziness, or blurred vision. - Have ever had an ectopic pregnancy or a history of ovarian cysts. Can I Become Pregnancy While Using Mirena?Although it is very rare, it is possible for you to become pregnant with Mirena in place. If you do not have your period at the normal time and have other symptoms of pregnancy (ex: nausea, tiredness, breast tenderness), you should see your doctor for an examination and pregnancy test. If you become pregnant with Mirena in place, you should have it removed as soon as possible. If it is left in place during pregnancy, the chances of having a miscarriage or premature delivery increase. The effect of levonorgestrel on a developing infant is not well known, therefore a detrimental effect cannot be completely ruled out. You may wish to consider termination of the pregnancy. Your doctor will advise you. What If I Want a Baby?If you want a baby, ask your doctor to remove Mirena. Your usual level of fertility will return very quickly after the system is removed. Nearly 90% of women wishing to become pregnant conceive within 24 months after the removal of the system. How is Mirena Inserted?Before inserting Mirena, your doctor will perform a pelvic examination to determine the position and size of your uterus. Following this, your doctor will insert a thin, flexible plastic tube containing Mirena into your uterus. At this point you may feel a little discomfort. Once Mirena is in the correct position, your doctor will withdraw the tube, leaving the system in place in the uterus. Finally, your doctor will trim the removal threads to a suitable length. After insertion you may feel some cramp-like menstrual pain; however, this usually disappears within a few days. Most women find that the insertion procedure causes minor discomfort; however, for some it might be more uncomfortable. If concerned, you may wish to discuss the need for a painkiller or local anesthetic with your doctor. Some women may feel faint after the system is inserted, but this feeling subsides after a short rest. In very rare cases, part or all of the system may penetrate the wall of the uterus during insertion and come to rest outside the uterus. If this happens, the system must be removed. When Should Mirena Be Inserted?The system should be inserted during your period or within 7 days of it starting. When replacing an existing system for a new one, it is not necessary to wait for your period. Following childbirth, Mirena should not be fitted until 6 weeks after delivery. How Long Does Insertion Take?The insertion procedure usually takes a few minutes after your doctor has completed the pelvic examination. How Quickly Does Mirena Start to Work?You will be protected from pregnancy as soon as insertion of the system is complete; however, it is best to wait 24 – 48 hours before having sexual intercourse. What About Side Effects?Menstrual bleeding irregularity, or of increased amount, are the most common side effects of Mirena during the first months after the system is inserted, but these effects should decrease over time. Apart from menstrual changes, other side effects might include lower abdominal pain, headache, acne or other skin problems, tender breasts, back ache, a feeling of sickness, or period pain. You should tell your doctor if you have lower abdominal (tummy) pain, especially if you have missed a period or have unexpected bleeding. This might be a sign of ectopic pregnancy. Ectopic pregnancy (development of a fertilized egg outside the uterus) is possible with Mirena, but is highly unlikely. The risk of this happening is lower than for women using no contraception. If you think you are reacting poorly to Mirena, or are having other problems, please tell your doctor. How Often Should I Have Mirena Checked?You should have the system checked approximately 6 weeks after it is fitted, again at 12 months and then once a year until it is removed. Mirena can stay in place for 5 years before it must be removed. You should see your doctor if: - You cannot feel the threads anymore. - You can feel the lower end of the system. - You think you are pregnant. - You have persistent abdominal pain, fever or unusual discharge from the v****a. - You or your partner feel pain or discomfort during sexual intercourse. - There are sudden changes in your menstrual periods; for example, your menstrual pains stop completely and then you have persistent bleeding or pain, or you have little or no menstrual bleeding and then you start bleeding heavily. - If you have other medical problems, such as migraine headaches or intense headaches that recur, sudden problems with vision, jaundice (a yellowing of the whites of the eyes or nails) or high blood pressure. How Can I Check if Mirena is in Place?After each menstrual period, or about once a month, you should check by feeling if the two threads are still in place. Your doctor will show you how to do this. Do not pull on the threads as you may accidently pull the system out. If you cannot feel the threads, go to your doctor and in the meantime use another method of contraception. You should also go to your doctor if you can feel the lower end of the system itself. Will Mirena Interfere With Sexual Intercourse?During sexual intercourse, you or your partner should not be able to feel Mirena. If you can feel Mirena, or if you feel any pain or discomfort that you suspect may be caused by it, then you should not have sexual intercourse until you see your doctor to verify it is still in the correct position. Can I Breast-feed While Using Mirena?Small quantities of levonorgestrel, the medicinal ingredient in Mirena, have been found of the milk of breast-feeding women using Mirena; however, there does not appear to be a detrimental effect on growth or development of breast-fed infants whose mothers started using the product 6 weeks after delivery. How Will Mirena Affect My Periods?Mirena will affect your menstrual cycle. You might experience frequent spotting (a small amount of blood loss) or light bleeding in addition to your periods for the first 3 – 6 months. In some cases, you may have heavy or prolonged bleeding during this time. Overall, you are likely to have a gradual reduction in the number of bleeding days and in the amount of blood loss each month. Some women using Mirena eventually find that their periods stop altogether. When the system is removed, periods return to normal. What If I Stop Having Periods?Gradually, over time, your menstrual period may disappear. This is because of the effect of the hormone on the lining of the uterus. The normal monthly thickening of the uterine lining with blood does not happen, therefore there is little or no bleeding as happen during a usual menstrual period. It does not necessarily mean you have reached menopause or are pregnant. Your own hormone levels remain normal. If however, you are having regular menstrual periods and then you do not have one for 6 weeks or longer, it is possible that you may be pregnant. You should speak to your doctor. Safe Sex: Does Mirena Protect Against Sexually Transmitted Diseases (STDs)?Mirena does not protect you against sexually transmitted diseases including HIV/AIDS. For protection against STDs, it is advisable to use a condom. Do Other Drugs Interfere With Mirena?You should tell your doctor if you are taking any other medications. Can Mirena Fall Out?It is unlikely, but possible, that Mirena can come out either completely or partially. If this happens, you are not protected against pregnancy. An unusual increase in the amount of bleeding during your period might be a sign that this has happened. You can check that Mirena is in place by feeling for the threads as explained by your doctor. If you think it has come out, use another method of contraception until you see your doctor. Removal of MirenaYou should see your doctor when you want to have Mirena taken out. You can do this at any time and removal is very easy; however, you should be aware that you may become pregnant upon removal of the system if you have had sexual intercourse during the previous week. Tell your doctor if you have had sexual intercourse during the previous week. ~ The information in this pamphlet is from Berlex Canada Inc. I do not claim to own any of this information, nor am I trying to profit from it.
|
 |
 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
 Posted: Sun Jun 28, 2009 9:55 pm Posted: Sun Jun 28, 2009 9:55 pm
Depo Provera (Injection)(From the old Birth Control Info Sticky) Depo-Provera - must get by prescription. - receive a hormone shot in your arm / buttocks every 12 weeks to: prevent release of the egg, thicken the cervical mucus to keep sperm from joining the egg, and prevent a fertilized egg from implanting in the uterus. Effectiveness: 99.7% effective - Not effective against STI's. Advantages: - protects against pregnancy for 12 weeks. - no daily pill. - nothing to put in place before intercourse. - can be used while breastfeeding (6 weeks after delivery). - can be used by some women who cannot take the Pill. - protects against cancer of the lining of the uterus, and iron deficiency anemia. Possible Problems: - side effects can include irregular bleeding and other discomforts, including weight gain, headaches, depression, and abdominal pain. - side effects cannot be reversed until medication wears off (up to 12 weeks). - may cause delay in getting pregnant after shots are stopped. ------------------- (From the old Depo Provera Info Sticky) Depo Info PamphletNow that you're using 4 times a year birth control, our Registered Nurses can remind you when to schedule your next appointment and answer all your questions. Dial 1 - 888 - 671 - DEPO (3376).Information for Women Considering The Use of Depo-Provera As a Contraceptive, or Who Are Already Using It for ContraceptionIntroductionREAD THIS PAMPHLET VERY CAREFULLY. It has been prepared to help you make an informed decision on whether or not to choose Depo-Provera as your method of conception control (contraception), and help you get this best results from this medicine. Even if you have already decided to use Depo-Provera, READ THIS PAMPHLET VERY CAREFULLY. It contains general information and directions about this medicine and should add to the advice from your health practicioner. This pamphlet [booklet] should not replace your health practitioner's adfice. They may have given you different directions. If so, follow their advice. Also, if you have any questions or concerns after reading this pamphlet, talk to your health practitioner. Please contact your health practitioner if any of the following apply: - If you do not understand any part of this pamphlet. - If you want further information on other contraceptive methods. - If you are concerned that you should not use Depo-Provera. Important!: Depo-Provera is one of the most effective ways to prevent pregnancy other than sterilization. Depo-Provera does not protect you against HIV infections (AIDS) and other sexually transmitted diseases. Latex or polyurethane condoms are recommended for this purpose.You are required to have 4 injections a year with this method of contraception. There is some risk associated with the use of any medication. Depo-Provera is no exception. If you are thinking of using Depo-Provera as a contraceptive, it is importnat that you understand the risks. Some of these risks may continue after youhave stopped using Depo-Provera. Discuss these risks with your health practicioner before taking Depo-Provera; only you can decide whether Depo-Provera is the best contraceptive choice for you. Your health practicioner is the best person to discuss the risks and benefits of Depo-Provera.This pamphlet, however, will help you understand the most important information. It will also explain how you can help your health practitioner prescribe Depo-Provera as safely as possible by providing your complete medical history, and by being alert for the earliest signs of any possible problems. Make your decision to use Depo-Provera for contraception carefully. Think about the long-term action of Depo-Provera; once you get an injection of Depo-Provera, you mugt wait 3 months or more for the effects to wear off. Consider other methods of contraception if you wish to become pregnant shortly, or if you think that irregular or complete lack of menstrual periods would upset you. Q & A SectionWhat is Depo-Provera?Depo-Provera is an injectable conception control agent (contraceptive) that is given as 150 mg of the hormone medroxyprogesterone acetate. Medroxyprogesterone acetate is a chemical similar to (but not the same as) the natural hormone progesterone that is produced by your ovaries during the second half of your mestrual cycle. Depo-Provera does not contain the hormone estrogen. One injection of Depo-Provera provides protection against pregnancy for three months. Therefore you must have one injection every 3 months (up to 13 weeks). How Does Depo-Provera Work?During the three months following an injection, Depo-Provera stops the ripening of eggs in the ovaries; that is, it stops ovulation (the monthly release of an egg by the ovaries). When there is no ripe egg to be fertilized by the sperm, pregnancy cannot occur. Depo-Provera changes the lining of the uterus (the endometrium) so that it does not easily receive a fertilized egg. It also causes thickening of the secretions (mucus) in the cervix, making it more difficult for the sperm to enter the uterus. How Effective is Depo-Provera?Depo-Provera is more than 99.7% effective for conception control. This means less than one pregnancy for every 100 women who use Depo-Provera for a year (exactly as directed). Depo-Provera has been used as a conception control method by over 30 million women in over 100 countries. Depo-Provera and oral contraceptives ("the Pill") are theoretically equally effective at preventing pregnancy. But in actual use, Depo-Provera is more effective because women sometimes forget to take their "pills". Depo-Provera is more effective than IUD's, condoms (sometimes called rubber sheaths or prophylactics), diaphragms, or other contraceptive methods shown in Table 1 below. Other Ways to Prevent PregnancyOther methods of contraception are available to you. Other than Depo-Provera, sterilization, Norplant and IUD's, how well other methods of contraception work depends in part on how reliably they are used. Faithful users may achieve pregnancy rates in the lower ranges; others may expect pregnancy rates more in the middle of the ranges, of those shown in Table 1 below. Table 1 shows the reported pregnancy rates for various forms of birth control, including no birth control. The reported rates represent the number of women out of 100 who would becoming pregnant during the first year of use.  Who Should Not Use Depo-Provera? Who Should Not Use Depo-Provera?Depo-Provera should not be used by certain women. Tell your heal practitioner if you have any of the following conditions; only your health practitioner can determine if you should use Depo-Provera: 1) If you are pregnant, or think you might be pregnant. 2) If you want to become pregnant shortly. 3) Unusual or unexplained vaginal bleeding that your health practitioner does not know about. 4) Lumps, swelling, or tenderness of the breast that your health practitioner does not know about. 5) Problems with your liver or liver disease (ie - hepatitis). 6) If you are currently taking anticoagulant (blood-thinning) medication (ie - warfarin). 7) If you are allergic to medroxyprogesterone acetate, or any of the other ingredients found in Depo-Provera (polythylene glycol, polysorbate 80, sodium chloride, methylparaben, proplyparaben, water for injection). What Should Your Health Practitioner Know?Tell your health practicioner if you or any immediate family member has ever had any of the following. Women with these conditions may need to be checked more often by their health practitioner if they choose Depo-Provera: - Breast cancer, abnormal breast exam or x-ray (mammogram) - Diabetes - Seizures, convulsions, epilepsy - Migraines (headaches) - Asthma - Problems with heart, heart attack - Stroke, blood clots (coagulation disorder) - Problems with kidneys - High blood pressure - Mental depression - Scanty or irregular menstrual periods Tell your health practitioner if you are taking, or begin taking any other medicines, even medicines you buy without a prescription. Some medicines may interfere with each other in your body. The Risks of Using Depo-Provera1) The Formation of Tumors.A long term examination of women using Depo-Provera shows no overall increased risk of ovarian, liver, or cervical cancer. The same examination showed a prolonged, protective effect of reducing the risk of endometrial cancer in the population of users. Women who have ever used Depo-Provera showed no increased risk of breast cancer. And overall, there was no increase in risk of breast cancer with increased duration of use of Depo-Provera. However, in a certain set of women, those who first took the drug within the previous 4 years and who were under 35 years of age showed a slight increase of breast cancer associated with use of Depo-Provera. 2) Use in Pregnancy.Do not use Depo-Provera if you are pregnant or if you think you might be pregnant. It will not prevent the pregnancy from continuing, but may interfere with the normal development of your baby. To reduce the risk of using Depo-Provera while you are pregnant, use your injection only within the first 5 days of the beginning of your normal menstrual period, or only within the first 5 days after giving birth if you are NOT breast-feeding. 3) Use While Breast-Feeding.Before using Depo-Provera while breast-feeding, discuss it with your health practicioner. Depo-Provera does not affect the amount or quality of your milk. Children, whose mothers used Depo-Provera while breast-feeding for about 6 months, show no harmful effects up to 14 - 16 years of age. There is no further information on these children past 16 years old. A very small amount of the medicine in Depo-Provera is transferred to the milk of nursing mothers. Discuss with your health practitioner, he/she can help you decide what is best in your situation. 4) Development of Osteoporosis.Depo-Provera may be a risk-factor for osteoporosis, similar to race, family history, low weight/height ratio, sedentary life style, and smoking. If you are considering using Depo-Provera, discuss with your health practitioner if you have any two of the following: - slim build - do not do any exercise - your bones are brittle (weak) - if you smoke. The Risks of Depo-Provera Compared to the Risks of Other Contraceptive MethodsThe risks of various methods of contraception have been analyzed to estimate the risk of death associated with each. This analysis has two parts: (a) the risk of the method itself, and (b) the risk of death due to pregnancy in the event that the method fails. A risk of death due to the method of contraception is associated with IUDs and oral contraceptives. However, the risk is low - less than the risk of death from childbirth. The exception is women over the age of 35 years of age who use "the pill" and smoke, where the risk of death is greater than that of childbirth. The estimated mortality rate of Depo-Provera is lower than that for IUDs, oral contraceptives or childbirth. What Can You Expect From Depo-Provera? Some women have side effects from this medicine. Remember, medicines affect different people in different ways. Just because side effects have occured in other women, this does not mean you will get them [and vice versa]. The side effect that occurs most often are changes in menstrual patterns (during treatment). 1) Changes in Menstrual Patterns.Depo-Provera slowly and continuously releases a hormone into your body for about three months. Because of this, you are not likely to have regular periods. For the first 3 - 6 months, most women have irregular, unpredictable or even continuous bleeding. This bleeding may be as heavy as a typical period, or it may be lighter. This unpredictable bleeding pattern may be inconvenient, but it is normal due to the change Depo-Provera causes in the lining of your uterus. The lining no longer thickens each month and therefore, does not need to be lost as menstrual flow. As you continue to use Depo-Provera, bleeding generally decreases until most women no longer have monthly periods by the end of the first year of use. The lack of bleeding is NOT a sign of pregnancy. After you stop using Depo-Provera, the uterine lining will start to thicken again. Periods will start again as soon as the effects of Depo-Provera completely wear off. The time this takes varies from woman to woman. Very heavy bleeding that persists for several days is NOT a normal effect of Depo Provera. If this happens, call your health practitioner immediately.2) Return of Fertility.Depo-Provera will not make you infertile. Because Depo-Provera is a long-acting method of contraception, it takes more time after the last injection for its effect to wear off. This varies from woman to woman. Most women, however, must wait from 6 - 8 months after the last injection to start ovulating, have regular periods, and be able to become pregnant. If you stop using Depo-Provera and you do NOT want to become pregnant, start using another method of contraception 3 months after your last injection of Depo-Provera. If you want to become pregnant, tell your practitioner. 54% of women who wish to become pregnant do so within 6 months of their last injection of Depo-Provera. 76% of all women become pregnant within 1 year, and 92% become pregnant within 2 years. The average time to pregnancy is 9 months after the last injection. Table 2 shows the percent of women that become pregnant after stopping the use of Depo-Provera, oral contraceptives, and IUDs. 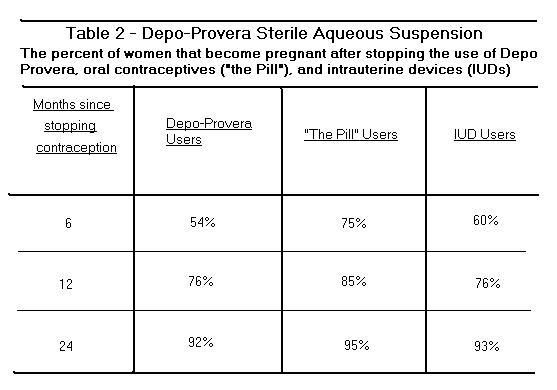 In rare cases, it can take two years or longer for ovulation and regular periods to return, and for you to be able to become pregnant. This delay in return of fertility (after stopping Depo Provera injections) is not related to how long Depo-Provera has been used. In very rare cases, women have not become pregnant after stopping injections of Depo-Provera. The reason is not known. There many reasons why women are unable to become pregnant, including increased age and the start of menopause. Im the general population, 7 out of every 100 women are unable to get pregnant. 3) Weight Gain.Some women gain weight due to an increased appetite while using Depo-Provera. If you notice a large increase in your weight (more than 15lbs or 7kg) in a short period of time that is not easily explained, tell your health practitioner. 4) Mental Depression.Women who have a history of depression may find that Depo-Provera will worsen this condition. If this happens to you or if you become depressed, tell your health practitioner. 5) Other Side Effects.Just as some women notice bodily changes before their period, you may notice some of the same changes after an injection of Depo-Provera. Although reported less often than changes in bleeding patterns, the following side effects have been reported in rare cases by some women. Tell your health practitioner right away if any of the following side-effects continue, bother you, or are not easily explained: - headaches - weight gain - nausea - vomiting - nervousness - stomach cramps - backache - depressed feeling - tiredness - dizziness - loss of hair from your head - increase in growth of body hair - vaginal dryness during sexual intercourse - bloating in the stomach - breast discharge and breast tenderness - spotty darkening of the skin - skin rashes - increase or decrease in sex drive - increase or decrease in blood pressure The injection itself may cause slight pain and a slight lump may appear under the skin. The lump will usually disappear in a few days. Other side effects which cannot be predicted may happen in rare cases. If you have any bothersome or unusual effects while using Depo-Provera, check with your health practitioner right away. How and When Should You Use Depo-Provera?After you have discussed the use of Depo-Provera with your health practitioner and have decided to use Depo-Provera. 1) Injections Every Three Months.Depo-Provera is injected into the muscle (for example, into the fleshy part of the hip [buttocks] or upper arm). For Depo-Provera to prevent you from getting pregnant, you must get an injection every 3 months (up to 13 weeks). This means you will have to schedule 4 injections a year. 2) The First Injection.If your bleeding pattern is unusual, have a pregnancy test before you receive your first injection. Do not use Depo-Provera if you are pregnant, or think you might be pregnant. It will not prevent the pregnancy from continuing, but may interfere with the normal development of your baby. For this reason, get your first injection only within the first 5 days from the beginning of your (menstrual) period, or only within the first 5 days after giving birth if you are NOT breast-feeding. Before using Depo-Provera while breast-feeding, discuss it with your health practitioner. When this procedure is followed, Depo-Provera will be effective from the day of injection. If Depo-Provera is given after the first 5 days of the beginning of your (menstrual) period, it may not prevent you from getting pregnant for the first 3-4 weeks after the injection. Use another non-hormonal contraceptive method (ie - condom, diaphram, sponge, cervical cap, abstinence, etc) during these 3 - 4 weeks. 3) Repeat Injections.See your health practitioner a week or two early if you know that it will be difficult to get your next injection three months after the last one. This contraceptive method does require you to plan ahead. If scheduling injections every three months would be difficult, then Depo-Provera is probably not the best contraceptive method for you. 4) If You Miss Your Injection of Depo-Provera.You can get your injection up to 13 weeks, or as early as 10 weeks, after your last injection. If you have not had your injection by the 13th week, you should have a pregnancy test done before any further injections. 5) Duration of Use.At the present time, no known reason exists to limit the time you can use Depo-Provera for contraception control [Nikolita's edit: Evidence exists now which contradicts this. Please see post 3 for more information]. No known medical reason exists for stopping its use periodically. If you continue to use Depo-Provera until you approach the usual age of menopause, ask your health practitioner when to stop using Depo-Provera. 6) Steps After Childbirth, Miscarriage, or Therapeutic Abortion (honestly that's what it says sweatdrop )If you plan to use Depo-Provera following childbirth, get your injection during the first five days after giving birth if you are NOT breast-feeding. If you choose to breast-feed, discuss with your health practitioner the possibility of getting pregnant, other possible contracepties, and when you may start using Depo-Provera (see previous information on "Use While Breast-feeding"). After miscarriage or therapeutic abortion, talk to your health practitioner about when you may start using Depo-Provera. 7) If You See a Different Health Practitioner.If you see a different health practitioner, tell him/her that you are using Depo-Provera. 8 ) If You Take Other Medications.Tell your health practitioner if you are taking, or begin taking, any other medicines, even medicines you buy without a prescription. Some medicines may interfere with each other in your body. Remind him/her you are taking Depo-Provera. ------------------------- (From the old Depo Provera Info Sticky) Technical Depo Information (leaflet)Depo-Provera: Medroxyprogesterone Acetate Injectable suspension, USP Sterile Aqueous Suspension Progestogen Action and Clinical PharmacologyDepo-Provera (medroxyprogesterone acetate) is a long-acting progestational steroid (progestogen) derived from a natural source (soy beans). Its long duration of action is a result of slow absorption from the injection site. Depo-Provera does not contain estrogen. For conception control, Depo-Provera inhibits the secretion of gonadotropins which, in turn, prevent follicular maturation and ovulation, and result in endometrial thinning. Additional progestational effects that may contribute to the contraceptive effectiveness of Depo-Provera include the transformation and maintenance of an endometrium hostile implantation, and thickening of cervical mucus making sperm penetration of the cervix more difficult. Depo-Provera administered parenterally to women with adequate endogenous estrogen transforms proliferative endometrium into secretory endometrium. The anti-cancer activity of Depo-Provera at pharmacologic doses may be dependent on its effect on the hypopituary gland/gonadal axis, estrogen receptors, and the metabolism of steroids at the tissue level. Following at a single 150 mg IM dose of Depo-Provera, medroxyprogesterone acetate (MPA) concentrations, measured by an extracted radioimmunoassy procedure, increase for approximately 3 weeks to reach peak plasma concentrations of 1 - 7 ng/ml. The levels then decrease exponentially until they become undetectable (<100 ng/ml) between 120 - 200 days following injection. Using an unextracted radioimmunoassy procedure for the assay of medroxyprogesterone acetate in serum, the apparent half-life for medroxyprogesterone acetate following IM administration of Depo-Provera is approximately 50 days. The principal metabolite of medroxyprogesterone acetate that has been identified is a 6a-methyl-6b [it's a symbol I don't have a character for, "b" comes closest], 17a, 21-trihydroxy-4 pregnene-3, 20-dione-17-acetate, which is excreted in the urine. The effect of hepatic and/or renal disease on the pharmacokinetics of Depo-Provera is unknown. Indications and Clinical UseDepo-Provera (medroxyprogesterone acetate) is indicated for: 1) Conception control (prevention of pregnancy). 2) Tratment of endometriosis. 3) Adjunctive and/or palliative treatment of recurrent and/or metastatic endometrial or renal cell carcinoma (hypernephroid carcinomas). 4) Adjunctive or palliative treatment of hormonally-dependent recurrent inoperable, or metastatic carcinoma of the breast in post-menopausal women. Contraindications [Not recommended for] Not for intravenous use.Depo-Provera (medroxyprogesterone acetate) is contraindicated [(of a symptom or condition) to give indication against the advisability of (a particular or usual remedy or treatment)] in women with: 1) Known or suspected pregnancy or as a diagnostic test for pregnancy. 2) Undiagnosed vaginal and/or urinary tract bleeding. 3) Undiagnosed breast pathology. 4) Thrombophlebitis, thromboembolic disorders, cerebral apoplexy, or women with a past history of these conditions. 5) Liver disfunction or disease. 6) Known hypersensitivity to Depo-Provera (medroxyprogesterone acetate or any of its other ingredients). Warning1) Irregular Menstrual Patterns.Disruption of menstrual patterns is common following the administration of Depo-Provera (medroxyprogesterone acetate). This includes irregular or unpredictable bleeding or spotting, or rarely heavy or continuous bleeding. If undiagnosed bleeding occurs, or if abnormal bleeding persists or is severe, appropriate investigation should be instituted to rule out the possibility of organic pathology, and appropriate treatment instituted if necessary. As women continue to use Depo-Provera, fewer experience irregular bleeding patterns and more experience amenorrhea [loss of menstrual period]. By month 12, amenorrhea was reported by 55% of women, and by month 24, amenorrhea was reported by 68% of women using Depo-Provera. Because of the prolonged effect following intramuscular injection of Depo-Provera, re-establishment of menstruationg may be delayed and difficult to predict. For this reason, Depo-Provera is not recommended for treatment of secondary amenorrhea or functional uterine bleeding. For these conditions, oral progestogen therapy is recommended. 2) Bone Mineral Density Changes.Depo-Provera may be a risk factor for osteoporosis, similar to race, family history, low weight/height ratio, sedentary life style, and smoking. Until further information is available, risk factors for osteoporosis should be reviewed and bone density measurements should be obtained for women with multiple risk factors, especially if the drug is being considered for long-term use. It may be advisable to consider alternative methods for women with bone density measurements in the lower normal range. Physiologically, although Depo-Provera slows the loss of bone density in premenopausal women due to its anabolic effects, in premenopausal women, it surpresses estrogen production which may lead to a loss of bone density. One study conducted in New Zealand showed a relative decrease in bone density in long-term users of Depo-Provera. The level of bone density decrease did not meet the criteria for diagnosis of osteoporosis (>2.5 standard deviations below the mean) and no fractures were reported. The effects appeared to be reversible upon discontinuation. Further prospective study, which is ongoing, is needed to clarify this issue. [For more information, go here] 3) Risk of Malignancy.Long-term case-controlled surveillance of users of Depo-Provera found slight or no increased overall risk of breast cancer, and no overall increased risk of ovarian, liver or cervical cancer and a prolonged, protective effectof reducing the risk of endometrial cancer in the population of users. The World Health Organization Study, a component of a pooled analysis, showed an increased RR of 2.19* (95% CI 1.23 to 3.89) of breast cancer associated with the use of Depo-Provera in women whose first exposure to drug was within the previous 4 years and who were under 35 years of age. However, this overall RR for women who have ever used Depo-Provera was only 1.2 (95% CI 0.96 to 1.52). *Note: A RR of 1.0 indicates neither an increased nor a decreased risk of cancer associated with the use of the drug, relative to no use of the drug. In the case of the subpopulation with a RR of 2.19, the 95% CI is fairly wide and does not include the value of 1.0, thus inferring an increased risk of breast cancer in the defined subgroup relative to nonusers. The value of 2.19 means that women whose first exposure to the drug was within the previous 4 years and who are under 35 years of age have a 2.19-fold (95% CI 1.23 to 3.89-fold) increased risk of breast cancer relative to nonusers. The National Cancer Institute reports an average annual incidence rate for breast cancer for US women, all races, age 30 - 34 years of 26.7 per 100,000. A RR of 2.19, thus, increases the possible risk from 26.7 to 58.5 cases per 100,000 women. The attributable risk, thus, is 31.8 per 100,000 women per year. A statistically insignificant increase in RR estimates of invasive squamous-cell cervical cancer has been associated with the use of Depo-Provera in women who were first exposed before the age of 35 years (RR 1.22 to 1.28 and 95% CI 0.93 to 1.70). The overall, nonsignificant relative rate of invasive squamous-cell cervical cancer in women who ever used Depo-Provera Contraceptive Injection was estimated to be 1.11% (95% CI 0.96 to 1.29). No trends in risk with duration of use or times since initial or most recent exposure were observed. 4) Thromboembolic Disorders.Before prescribing Depo-Provera, the physician should be alert to the earliest manifestations of thrombotic disorders (thrombophlebitis, cerebrovascular disorders, pulmonary embolism, and retinal thrombosis). Should any of these occur or be suspected, the drug should be discontinued immediately. 5) Ocular Disorders.Discontinue medication pending examination if there is a sudden partial or complete loss of vision, or if there is a sudden onset of proptosis, diplopia or migraine. If examination reveals papilledema or retinal vascular lesions, medication should be withdrawn. 6) Return of Fertility.There is no evidence that Depo-Provera (medroxyprogesterone acetate) causes infertility. A large study of return of fertility shows that women conceived 9 months on average after the last injection, or 5.5 months after discontinuing (discontinuance is assumed to be 15 weeks after the last injection). In addition, the number of users who had conceived within 2 years of discontinuing their method of contraception (92% of Depo-Provera users had conceived within two years of discontinuing, compared with 93% for users if the IUD and 95% for uers of oral contraceptoves) were comparable. Discuss this information with women who intend to conceive in the next 1 - 2 years. In some cases women have not become pregnant after stopping injections of Depo-Provera. It is not known whether Depo-Provera or other factors resulted in a change in the ability to conceive. Many factors exist for such changes, including increased age and the onset of menopause. The infertility rate in the normal population is 7%. 7) Administration During Pregnancy.To increase assurance that the woman is not pregnant at the time of the first administration, it is recommended that the first injection be given only within the first 5 days of the onset of a normal menstruation period, or, only within the first 5 days post-partum if not breast-feeding. If the woman has chosen to breast-feed, discuss the risk of pregnancy and possible risks of Depo-Provera to determine the most appropriate course of action for the individual woman. (See Warnings: During Lactation: Dosage and Administration) Infants from unexpected pregnancies that occured 1 - 2 months after injection of Depo-Provera may be at an increased risk of low birth weight, which, in turn, is associated with an increased risk of neonatal death. The attributable risk is low because such pregnancies are uncommon. A significant increase in incidence of polysyndactyly and chromosomal anomalies was observed among infants of users of Depo-Provera, the former being most pronounced in woman under 30 years of age. The unrelated nature of these defects, the lack of confirmation from other studies, the distant preconceptual exposure to Depo-Provera and the chance effects due to multiple statistical comparisons, make a casual association unlikely. Children exposed to medroxyprogesterone acetate in utero and followed to adolescence showed no evidence of any adverse effects on their health, including their physical, intellectual, sexual or social development. Several reports suggest an association between intra-uterine exposure to progestational drugs in the first trimester of pregnancy and genital abnormalities in male and female fetuses. The risk of hypospadias (5 - 8 per 1,000 births in the general population) may be approximately doubled with exposure to these drugs. Although there are insufficient data to quantify the risk to exposed female fetuses, some of these drugs induce mild virilization of the external genitalia of the female fetus. Because of these changes, it is prudent to avoid the use of progestogens during the first trimester of pregnancy. 8 ) During Lactation.Detectable amounts of progestogen have been identified in the milk of mothers receiving Depo-Provera. Two studies have indicated that the maximum amount of medroxyprogesterone acetate (MPA) which might be ingested by a breast-feeding infant whose mother is receiving Depo-Provera for contraception would be 1.0 - 1.5 [unit untypeable]/day (or 0.0015 mg/day, 0.045 mg/month, 0.27mg over 6 months, which is is about 0.05 mg/kg over 6 months for a 5.5 kg baby). If absorption properties between between adult and infant are comparable, this amount would be too low to suppress pituitary function in the infant. No adverse effects related to lactation itself or infant growth were reported in studies where Depo-Provera was started 1 - 4 days, 7 days or within 6 weeks post-partum. In nursing mothers treated with Depo-Provera, milk composition, quality and amount were not adversely affected. To date, no adverse effects have been observed in children whose mothers were using Depo-Provera while lactating. A study of children exposed to MPA with median observation periods of 14 - 16 years, indicated no incidence of adverse effects on physical growth, mental growth, and development of general health status. However, the long-term effects on the child are not fully understood. The physician and woman should discuss the risks of pregnancy versus the risks to the child, if Depo-Provera is used during lactation, to determine the most appropriate course of action for the individual woman. 9) Ectopic Pregnancy.Physicians should investigate the possibility of an ectopic pregnancy among women using Depo-Provera who complain of severe abdominal pain. 10) Anaphylactic Reaction.Anaphylactic and anaphylactoid reactions have occasionally been reported in women treated with Depo-Provera. If an anaphylactic reaction occurs, appropriate therapy should be instituted. Serious anaphylactic reactions require emergency medical treatment. 11) Adrenocortical Function.Clinical suprpression of adrenocortical functions has been been observed at low dose levels used for contraception (ovulation suppression). However, at very high doses (500 mg daily or more) used in the treatment of certain cancers, corticoid-like activity has been reported. 12) Cushingoid Symptoms.The high doses of Depo-Provera used in the treatment of cancer may, in some cases, produce Cushinoid symptoms (ie - moon faces and blood pressure elevation). PrecautionsI) General.1) Pretreatment Examination.Before using Depo-Provera, a thorough history and physical examination -including breasts, liver, pelvic organs, blood pressure determination, and Papanicolaou smear - should be performed. Periodic follow-up examinations should be conducted and include all procedures done at the initial visit. 2) Hepatic Function.Liver function tests should be performed periodically in women who are suspected of, or who are at risk of, having hepatic disease. The physician should be alert to the earliest manifestations of the impaired liver function. Should this occur or be suspected, the treatment should not be continued. The woman's status should be re-evaluated at appropriate intervals. If jaundice develops, consideration should be given to discontinue the drug. 3) Carbohydrate Metabolism.A decrease in glucose tolerance has been observed in some women receiving Depo-Provera (medroxyprogesterone acetate). The mechanisms of this decrease is obscure. For this reason, diabetic women should be carefully observed while receiving Depo-Provera. 4) Cardiovascular Function.Medroxyprogesterone acetate has not been shown to affect coagulation and has been associated only rarely with cardiovascular incidents (ie - medullary infarction in a heavy smoker). 5) Fluid Retention.Since progestogens may cause some degree of fluid retention, conditions that might be influenced by this factor, such as epilepsy, migraine, asthma, or cardiac or renal dysfunction, require careful observation. 6) CNS Disorders and Convulsions.Women who have a history of mental depression should be carefully observed and this drug discontinued if serious depression re-occurs. Some women may complain of premenstrual-like depression while on Depo-Provera therapy. There have been few reported cases of convulsions in patients who were treated with Depo-Provera. Associatino with Dep-Provera use of pre-existing conditions is not clear. 7) Weight Changes. Weight gain may be associated with the use of Depo-Provera. (See Adverse Reactions) 8 ) Age.The age of the woman constitutes no absolute limiting factor although treatment with a progestogen may mask the onset of the climacteric. 9) Laboratory Tests.Certain endocrine and possibly liver function tests may be affected by treatment with Depo-Provera. Therefore, if such tests are abnormal in a woman taking Depo-Provera, it is recommended that they be repeated 6 - 12 months after the drug has been withdrawn. The clinical chemist or pathologist should be advised of progestogen therapy when a woman's blood or tissue specimens are submitted for laboratory diagnosis or biochemical analysis. The following laboratory tests may be affected by the use of Depo-Provera: (a) Gonadotropin levels - inhibition of the midcycle LH surge. (b) Plasma progesterone levels - inhibition of ovulation and this the postovulatory rise of progesterone. (c) Plasma estrogen levels - do not exceed early-to-mid-proliferative phase levels. (d) Plasma cortisol levels - not significantly affected by the dose used for contraception. (e) Glucose tolerance test - occasionally some degree of glucose intolerance may develop. (f) Metyrapone test - modest depression of response to metyrapone test. (g) Plasma lipid concentrations - decrease in high density lipoprotein cholesterol (HDL-C) in some studies. The clinical relevance of this has yet to be determined. (h) Urinary pregnanediol levels (Note: Depo-Provera does not interfere with the assay of human chorionic gonadptropin [HCG] either chemically or pharmacologically). II. For Conception Control.1) Counselling. It is very important that adequate explanations of the long-term nature of Depo-Provera as a contraceptive be given to each woman prior to her first injection. The possible side effects including changes in menstrual cycle and the relatively slow return of fertility should be emphasized. Every effort should be made to ensure that each woman receives such counselling as to enable her to understand fully these explanations and the possible consequences. A detailed supplementary information booklet that describes the actions, benefits, risks, and adverse effects of this contraceptive should be made available to each woman before she makes the decision to use Depo-Provera as conception control.2) Sexually Transmitted Diseases [STDs].Women should be counselled that this product offers no protection from the acquisition of sexually transmitted infections, including HIV, and that latex or polyurethane condoms are recommended for this purpose.3) Follow-up Examination.The first follow-up examination should be made within 6 months after Depo-Provera is prescribed, and therefore at least once a year. At each annual visit, the examination should include all procedures done at the initial visit. The women must return every 10 - 13 weeks for a repeat injection to maintain contraception effectiveness (see "Dosage and Administration"). If an injection is not given within 13 weeks, a pregnancy test should be done before any further treatment with Depo-Provera. 4) Weight Changes. The majority of studies report a mean weight gain of 5.4 lbs (2.5 kg) at the end of one year, but only 2% of women discontinued treatment due to excessive weight gain (See "Adverse Reactions: Clinical Trials"). Many studies indicate that weight gain occurs mainly in the first year of use, however, others do report a slow and continuing increase which may reach a mean of 8 lbs (3.6 kg) by the end of two years. Some 20 - 40% of Depo-Provera users actually lose weight during treatment. Adverse ReactionsThe following adverse reactions have been associated with the use of Depo-Provera. (A) Irregular Menstrual Patterns.The most common adverse reactions associated with the use of Depo-Provera for conception is the disruption of menstrual patterns. his includes irregular or unpredictable bleeding or spotting, or rarely heavy or continuous bleeding. In U.S. studies of 3,905 women receiving Depo-Provera every 3 months, unpredictable bleeding or spotting were commonly reported during the first few menstrual cycles with frequency, duration and amount of bleeding diminishing gradually. By mont 12, amenorrhea was reported by 55% of the women, and by month 24, amenorrhea was reported by 68% of the women using Depo-Provera. Bleeding or spotting persisted for more than 10 days of the month in about 12% of the users. And abnormally or prolonged bleeding occurs in about 1 - 2% of users (See "Clinical Trials"). (B) Non-Menstrual Adverse Reactions.Other than menstrual changes, weight gain, headache and abdominal discomfort are the most common side effets. The U.S. studies of 3,905 women receiving Depo-Provera every 3 months report a mean weight gain of 5.4 lbs (2.5 kg) at the end of one year, but only 2% of women discontinued treatment due to excessive weight gain (See "Adverse Reactions: Clinical Trials"). Many studies indicate that weight gain occurs mainly in the first year of use, however, others do report a slow and continuing increase which may reach a mean of 8 lbs (3.6 kg) by the end of two years. Some 20 - 40% of Depo-Provera users actually lose weight during treatment. In a few instances, there have been undesirable sequelae at the site of injection, such as a residual lump, chnage in colour of the skin, or a sterile abscess. Anaphylactic and anaphylactoid reactions have been reported on rare occasions. The occurance rates for non-menstrual adverse reactions reported in U.S. studies of 3,905 women receiving Depo-Provera every 3 months are listed below. 2,253 women were in the study for 12 months or more, 827 women were in the study for 36 months or more. The total number of patient-months of experience was 82,384. A total of 2,117 of the 3,905 women (54%) reported no side-effects. Allergic:- Allergic reactions, hives (0.2 - 1.0%) Cardiovascular:- Chest pain, tachycardia (0.2% - 1.0%) Central Nervous System:- Headache (17%) - Nervousness (12%) - Dizziness (6%) - Depression (2%) - Insomnia, pain, somnolence or drowsiness (0.2 - 1.0%) Dermatologic:- Acne, alopecia, rash (1%) Endocrine:- Decreased libido (6%) - Breast swelling/tenderness (3%) - Hot flashes (1%) - Galactorrhea, chloasma, hirsutism (0.2 - 1.0%) Gastrointestinal:- Abdominal distress (12%) - Nausea (4%) - Bloating (2%) - Anorexia, increased appetite, diarrhea, heartburn, abdominal swelling, vomiting, constipation (0.2 - 1.0%). Gynecologic/Urologic:- Vaginal discharge (3%) - Dysmenorrhea (2%) - Pruritus vulvae (1%) - Genitourinary infection, dysuria, bleeding requiring D&C, dyspareunia, urinary frequency (0.2 - 1.0%) Hepatic:- Liver disorders, NOS, altered liver function (0.2 - 1.0%) Metabolic:- Peripheral edema (2%) Musculoskeletal:- Backache (2%) Neurologic:- Asthenia (5%) - Limb pain (4%) - Pruritus, paraesthesia or sensory disturbances (0.2 - 1.0%) Respiratory:- Dyspnea (0.2 - 1.0%) Special Senses:- Eye discomfort (0.2 - 1.0%) Symptoms and Treatment of OverdosageOverdose may result in a period of amenorrhea of a variable length and may be followed by ireegular menses for several months. There is no known therapy for overdose. Dosage and AdministrationDepo-Provera (medroxyprogesterone acetate) is intended for INTRAMUSCULAR ADMINISTRATION ONLY. Immediately before use, the sterile aqueous suspension should be vigoriously shaken to assure that the dose being administered represents a uniform suspension. Conception Control (Contraception)The recommenddd dose for contraception is 150 mg of Depo-Provera every 3 months, administered by deep intramuscular injection. To increase assurance that the woman is not pregnant at the time of the first administration, it is recommended that this injection be given only within the first 5 days of the onset of a normal menstrual period, or, only within the first 5 days post-partum if not breast-feeding. If the woman has chosen to breast-feed, discuss the risks of pregnancy and possible risks of Depo-Provera to determine the most appropriate course of action for the individual woman (See "Warnings"). If administered within the first 5 days after the onset of a normal menstrual period, Depo-Provera is effective from the day of injection [Nikolita's edit: Effective after 24 hours, really. Better to be safe than sorry.]. When Depo-Provera is given later in the menstrual cycle, it may not be effective for the first 3 - 4 weeks after the injetion and another method of contraception (non-hormonal) should be used during this time. After miscarriage or first trimester therapeutic abortion, the injection is normally given within the first 5 days of the procedure and no extra precautions are required. After a late (second trimester) abortion, some further delay is recommended to reduce the risk of heavy and prolonged bleeding, therefore, the first injection should not be given until 4 weeks after the procedure. Intervals between injections must not exceed 13 weeks (3 months).EndometriosisThe recommended dose of Depo-Provera is 50 mg weekly, or 100 mg ever 2 weeks intramuscularly for at least 6 months. It should be noted that return of ovulation may be delayed following this therapy due to the depot properties of the drug (See "Warnings"). Endometrial and Renal CarcinomaDoses of 400 mg to 1,000 mg of Depo-Provera intramuscularly per week are recommended initially. If improvement is noted within a few weeks or months and the disease appears stabilized, it may be possible to maintain improvement with as little as 400 mg per month. Depo-Provera is not recommended as a primary therapy, but as adjunctive and palliative treatment in advanced, inoperable cases including those with recurrent or metastatic disease. Breast CancerThe recommended dosage schedule is Depo-Provera 500 mg/day intramuscular for 298 days. The woman should then be placed on a maintenance schedule of 500 mg twice weekly as long as she is responding to treatment. A response may not be evident until 8 - 10 weeks of therapy. If a rapid progression of the disease occurs at any time during therapy, Depo-Provera should be terminated. Pharmaceutical InformationDrug SubstanceProper name: Medroxyprogesterone acetate injectable suspension USP. Chemical name: (1) Pregn-4-ene-3,20 dione, 17-(acetyloxy)-6-menthyl-,(6a)-; (2) 17-Hydroxy-6a-menthylpregn-4-ene-3,dione acetate [Nikolita Edit: There's pictures and exponents for the Structural Formula, Molecular Formula and Molecular Weight that I can't type out. Try asking your doctor/gyno if you need the information.]Description: Medroxyprogesterone acetate is a white to off-white, odourless crystalline powder, stable in air. It is freely soluble in chloroform, soluble in acetate and dioxane, sparingly soluble in ethanol and methanol, slightly soluble in ether and insoluble in water. The melting point is between 200 and 210 degrees Celcius. The c log P is 1.467. [Nikolita's edit: There's a chat for the drug's composition. I won't post it unless someone asks for it, since it would take awhile to copy out. If you'd like to see it, please PM me and ask. 3nodding ]Stability and StorageProtect from freezing. Store at controlled room temperature 15 - 30 degrees Celcius. Shake well before using.
|
 |
 |
|
|
|
|
|
|
|
|
|
|
|
|
 Posted: Sun Jun 28, 2009 9:58 pm Posted: Sun Jun 28, 2009 9:58 pm
Depo Provera (Injection) - Additional Information(From the old Depo Provera Info Sticky) Additional Depo Provera InformationI can't confirm this 100%, but it's what the female doctor at the local clinic I visit said. Apparently Depo Provera can't be taken as a form of contraception past the 2 year mark. Once the 2 year mark passes, the woman must find another form of birth control to use. I wasn't clear if this was because the effects may become irreversible (which I was already aware of) or because it just stops being effective, but it's something to check with your doctor/gyno if you're considering taking Depo Provera. ---------- ---------- Please note: This article is from June. 2005, so the information is a little old, but the warning still stands true and most doctors should be aware of it by now.~ Taken from: http://www.hc-sc.gc.ca/dhp-mps/medeff/advisories-avis/public/2005/depo-provera_pa_ap_e.html KIRKLAND, QUEBEC - June 30, 2005 - Pfizer Canada Inc. in consultation with Health Canada, would like to inform you of important updated safety information for DEPO-PROVERA (medroxyprogesterone acetate injectable suspension, USP), indicated for conception control (prevention of pregnancy), treatment of endometriosis (tissue of the uterus abnormally growing outside of the uterus), treatment of recurrent and/or metastatic endometrial cancer (cancer of the lining of the uterus) or renal cell cancer (kidney cancer) and treatment of recurrent inoperable or metastatic breast cancer in post-menopausal women. As a result of new clinical studies, one with premenopausal adult women (age 25-35 years) and one with adolescent women (age 12-18 years) using DEPO-PROVERA for conception control, data regarding the use of DEPO-PROVERA and its associated effect on bone mineral density are now available. The data indicate that women who use DEPO-PROVERA may lose significant bone mineral density. The longer DEPO-PROVERA is used, the more bone mineral density may be lost. Bone mineral density may not return completely once use of DEPO-PROVERA has been discontinued. This is of particular concern when DEPO-PROVERA is used in adolescence (teenager years) when bone mineral density should instead be increasing. Loss of bone mineral density can cause osteoporosis (decrease in bone mass and density) and increase the risk that bones might break, especially after menopause (the end of menstrual periods).There have been cases of osteoporosis and fracture (broken bones) associated with the use of DEPO-PROVERA. Patients should be aware that DEPO-PROVERA should be used as a birth control method or endometrial treatment only if other treatments have been considered to be unsuitable or unacceptable and should be used for the shortest period of time possible. The risks and benefits of treatment should be carefully re-evaluated on a regular basis in all users of this drug. DEPO-PROVERA should not be used before menarche (the onset of menstrual periods). Patients should inform their doctor if they use any other medications (including steroids or anti-seizure medications), have a history of bone disease or anorexia nervosa (an eating disorder), have a strong family history of osteoporosis, drink alcohol or smoke. These conditions represent additional risk factors for low bone mineral density. Patients should talk to their doctor about how to reduce the risk of low bone mineral density, and about calcium and vitamin D intake. Patients should be aware that monitoring of bone mineral density with a bone test may be recommended for some users of DEPO-PROVERA. This public advisory is in addition to a letter issued to health care professionals reminding them of the above-mentioned safety information. As well, the product monograph for DEPO-PROVERA has been revised to inform doctors and other healthcare professionals regarding additional guidance on the appropriate use of DEPO-PROVERA. For more information about the revisions to the prescribing information, patients should consult their healthcare professional. Patients should NOT discontinue their medication without consulting their doctor first. For media inquiries, please contact Sophie McCann, Pfizer Canada Inc, (514) 693-4161. The safety of patients is a priority for Pfizer Canada Inc. Information about adverse drug reactions is gathered by both Pfizer Canada Inc. and Health Canada, via its Canadian Adverse Drug Reaction Monitoring Program (CADRMP). Any suspected adverse drug reactions in patients receiving Depo-Provera can be reported to: Pfizer Canada Inc. Safety and Medical Information P.O. Box 800 Pointe-Claire, Quebec H9R-4V2 1-800-463-6001 Any suspected adverse reaction can also be reported to: Canadian Adverse Drug Reaction Monitoring Program (CADRMP) Marketed Health Products Directorate HEALTH CANADA Address Locator: 0701C OTTAWA, Ontario, K1A 0K9 Tel: (613) 957-0337 or Fax: (613) 957-0335 To report an Adverse Reaction, consumers and health professionals may call toll free: Tel: 866 234-2345 Fax: 866 678-6789 cadrmp@hc-sc.gc.ca For other inquiries, please refer to contact information: Bureau of Metabolism, Oncology and Reproductive Sciences (BMORS) E-mail: bmors_enquiries@hc-sc.gc.ca Telephone: (613) 941-3171 Fax: (613) 941-1365 ~ LorienLlewellyn "There is no antidote to the Depo Provera shot. Women who are given Depo Provera should be well informed about the drug and know that there are other options for birth control. In this country and in other countries, women have been pressured into taking Depo Provera without knowing what it was. Know your options." http://www.fwhc.org/birth-control/bcdepo.htm
|
 |
 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
 Posted: Sun Jun 28, 2009 10:06 pm Posted: Sun Jun 28, 2009 10:06 pm
Norplant (Implant in the arm)(From the old Birth Control Info Sticky) Norplant (Implant) - must be obtained by prescription. - 6 small capsules inserted under the skin of your upper arm. - capsules constantly release small amounts of hormone that: prevent release of an egg, and thicken the cervical mucus to keep sperm from joining with the egg. - removal can be done at any time but only by a clinician. Effectiveness: 99.6% - Not effective against STI's. Advantages: - protects against pregnancy for 5 years. - no daily pill. - nothing to put in place before intercourse. - can be used while breastfeeding (6 weeks after delivery). - can be used by some women who cannot take the Pill. Possible Problems: - side effects can include irregular bleeding and other discomforts, including headaches, depression, and weight gain. - minor medical procedure needed for insertion and removal. - rarely, infection at insertion site. -------------------- Taken from: http://femmesensante.ca/centres/sex/birthcontrol/norplant.htmlNorplant is implanted in the inner upper arm as six tiny rods. They can remain in place and protect you from pregnancy for up to five years. Norplant is over 99 percent effective against pregnancy but it does not protect you from sexually transmitted infections. Norplant contains a progestin similar to one of the hormones that control a woman's menstrual cycle. When a woman uses Norplant: - her ovaries stop releasing eggs - the mucus in her cervix gets thick making it harder for sperm to enter - the lining of the uterus gets thinner making it hard for a fertilized egg to attach to the wall How to Use NorplantNorplant must be inserted in a clinic or a doctor's office. Before you have Norplant implanted, check whether your doctor or clinic will remove the rods at a later date. Some physicians do not do removals or charge extra for the removal. The underside of your arm is numbed but you remain awake for the procedure. A tiny incision is made and the rods are inserted in a fan shape. This takes 15 to 20 minutes and can be covered with a bandage. When it is healed you can't see the rods (unless you are very thin) but you can feel them under the skin. You should use another method of birth control as back up for a full week after insertion. After three months, return to your doctor or clinic for a check-up then continue to have your regular check-ups. To make sure you are not pregnant, Norplant should be inserted: - during your period - within seven days of an abortion - at least six weeks after the birth of a child (Once you have successfully started breast-feeding, Norplant is safe and will not interfere with your production of breast milk.) Norplant must be removed after five years but it can be removed sooner if you have side effects or wish to get pregnant. This may take slightly longer than having the rods inserted. Your arm may be painful for a few days. Your arm is numbed with an injection before the rods are removed. Advantages- very effective - periods may be lighter - may decrease menstrual cramps or pain - may help control the pain associated with endometriosis - can be rapidly reversed - you don't have to interrupt sex - the woman controls this method of birth control - can remain in place for five years - you don't have to remember a daily pill Disadvantages- expensive (around 500 dollars) - does not protect against sexually transmitted infections - may cause irregular bleeding - must be removed at a clinic or by a doctor - an infection in your arm is possible - sometimes difficult to remove - some women can't use Norplant You shouldn't use Norplant if you are pregnant, have abnormal vaginal bleeding, liver diseases such as jaundice or hepatitis, or breast cancer. Norplant is less effective if you weigh over 200 pounds or are taking some anti-seizure medications or antibiotics. If you are taking these drugs temporarily, you should use a back-up form of birth control for at least a week. The side effects of Norplant are very similar to the side effects associated with Depo-Provera. If these side effects interfere with your life you may wish to consider other methods of birth control. Women on Norplant may experience: - irregular menstrual bleeding - moodiness - irritation around the implant in your arm - weight gain (uncommon) -------------------- - More information on Norplant: http://en.wikipedia.org/wiki/Norplant (Wikipedia) **Includes information on why Norplant is no longer available in the US!**
|
 |
 |
|
|
|
|
|
|
|
|
|
|
|
|
 Posted: Sun Jun 28, 2009 10:18 pm Posted: Sun Jun 28, 2009 10:18 pm
Non-Hormonal Methods of Birth Control
(From the old Birth Control Info Sticky)
Lea Contraceptive
- is a shallow silicon cup.
- must be used with spermicidal jelly.
- can be purchased from a pharmacist without a prescription.
Effectiveness: 86% - 94% - Not effective against STI's.
Advantages:
- no major health concerns.
- no additional gel required within the first 8 hours of use.
- can be left in place up to 48 hours.
- a good alternative for those who have latex allergies.
- one size fits all.
Possible Problems:
- expensive.
- may be difficult to insert.
~
More information on the Lea Contraceptive:
- http://www.sexualityandu.ca/parents/contraception-2-12.aspx
- The cervical cap: http://en.wikipedia.org/wiki/Cervical_cap (Wikipedia)
-----------------------
(From the old Birth Control Info Sticky)
Diaphram or Cervical Cap
- must be fitted by a clinician.
- is a shallow latex cup (diaphram) or a thimble-shaped latex cup (cervical cap).
- must be used with spermicidal jelly, to prevent the sperm from joining with the egg.
Effectiveness: 82 - 94% effective - Not effective against STI's.
Advantages:
- no major health concerns.
- can last several years, if cared for correctly.
Possible Problems:
- can be messy.
- allergies to latex or spermicide.
- cannot use during vaginal bleeding or infection.
- diaphram: increased risk of bladder infection.
- cervical cap: difficult for some women to use, difficult to fit for some women.
~
More info on the diaphram and cervical cap:
- The diaphram: http://en.wikipedia.org/wiki/Diaphragm_(contraceptive) (Wikipedia)
- Diaphram info: http://www.sexualityandu.ca/adults/contraception-2-10.aspx
- The cervical cap: http://en.wikipedia.org/wiki/Cervical_cap (Wikipedia)
- Cervical cap info: http://kidshealth.org/teen/sexual_health/contraception/contraception_cap.html
----------------------
(From the old Birth Control Info Sticky)
Vaginal Spermicides
- made of chemicals that immobilize or kill sperm.
- create a barrier that sperm cannot penetrate.
- come as contraceptive foams, gels, film, suppositories and in sponges.
- can be purchased in pharmacies.
- are most effective when used with sponges.
~
More info on spermicides:
- Spermicides: http://en.wikipedia.org/wiki/Spermicide (Wikipedia)
- Vaginal spermicide info: http://www.medterms.com/script/main/art.asp?articlekey=9762
- Vaginal spermicide info: http://healthcenter.ucdavis.edu/topics/contraception/spermicides.html
------------------------
(From the old Birth Control Info Sticky)
Contraceptive Sponge
- is a polyurethane foam filled with F5 Gel (2 low dose spermicides).
- fits into the v****a easily.
- insert just prior or up to 1 hour before sex.
- F5 Gel covers walls of v****a and is released during intercourse.
- can be left in for 12 hours.
- can be used with a condom for extra protection.
~
More info on contraceptive sponges:
- Contraceptive sponge: http://en.wikipedia.org/wiki/Contraceptive_sponge (Wikipedia)
- Contraceptive sponge info: http://www.youngwomenshealth.org/femalebarrier3.html
|
 |
 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
 Posted: Sun Jun 28, 2009 10:32 pm Posted: Sun Jun 28, 2009 10:32 pm
Why the Pull-Out Method is NOT An Effective Form of Birth Control
(Thank you to unknwndreamer for providing some of these links and some of this information in the old Birth Control Info Sticky! biggrin )
Taken from: http://www.afraidtoask.com/contraception/bwithdrawal.html
History / How it works:
The man withdraws his p***s from the woman's v****a before ejaculation.
Summary of Withdrawal Method Effectiveness (Failure Rate)
Reportedly to be 79% effective, but statistical sample may not be adequate (e.g., likely is less effective in general population)
Benefits
- Better than nothing at all
- Inexpensive and requires no supplies
Risks
- Requires great self-control on the man's part
- Man must be able to predict exactly when he is going to ejaculate and therefore is difficult in men who ejaculate prematurely
- Even when p***s is withdrawn before ejaculation, pre-ejaculate often contains sperm (which means you can get pregnant)
- Be prepared to get pregnant and possibly catch a sexually transmitted disease
STD Protection
Absolutely none.
Cost
Free
-------------------------
Taken from: http://www.plannedparenthood.org/health-topics/birth-control/withdrawal-pull-out-method-4218.htm
Withdrawal at a Glance
- Withdrawal is also called coitus interruptus or the "pull out method"
- Something you can do during vaginal intercourse to prevent pregnancy
- Safe, easy, and convenient
Is Withdrawal for Me?
All of us who need birth control want to find the method that is best for us. And everyone has different needs when choosing a method. Whether you're thinking about using the pull out method, you're using the pull out method, or you're just someone who's curious about it, you may have many questions.
Here are some of the most common questions we hear people ask about withdrawal, or the pull out method. We hope the answers help you decide if it is right for you.
1) What Is Withdrawal?
A man who performs withdrawal will pull his p***s out of the v****a before ejaculation — the moment when semen spurts out of his p***s. Withdrawal is also known as coitus interruptus and the pull out method.
Withdrawal may be the world's oldest way to practice birth control. About 35 million couples worldwide rely on withdrawal.
2) How Does Withdrawal Work?
Withdrawal prevents pregnancy by keeping sperm out of the v****a. Pregnancy cannot happen if there is no sperm present.
3) How Effective Is Withdrawal?
Effectiveness is an important and common concern when choosing a birth control method. Like all birth control methods, the pull out method is much more effective when you do it correctly.
- Of every 100 women whose partners use withdrawal, 4 will become pregnant each year if they always do it correctly.
- Of every 100 women whose partners use withdrawal, 27 will become pregnant each year if they don't always do it correctly.
Couples who have great self-control, experience, and trust may use the pull out method more effectively. Men who use the pull out method must be able to know when they are reaching the point in sexual excitement when ejaculation can no longer be stopped or postponed. If you cannot predict this moment accurately, withdrawal will not be as effective.
Even if a man pulls out in time, pregnancy can still happen. Some experts believe that pre-ejaculate, or pre-c**, can pick up enough sperm left in the urethra from a previous ejaculation to cause pregnancy. If a man urinates between ejaculations before having sex again, it will help clear the urethra of sperm and may increase the effectiveness of withdrawal.
Pregnancy is also possible if semen or pre-ejaculate is spilled on the vulva.
Keep in mind that the withdrawal method does not protect you from sexually transmitted infections. Use a latex condom or female condom to reduce the risk of infection.
4) How Safe Is Withdrawal?
Anyone can use withdrawal safely — there are no side effects. [Like with hormonal birth control methods.]
5) What Are the Benefits of Withdrawal?
The pull out method is safe, simple, and convenient. Women and men like it because:
- It can be used to prevent pregnancy when no other method is available.
- There are no medical or hormonal side effects.
- No prescription is necessary.
- It is free.
The pull out method can also make other forms of birth control, such as the cap, condom, diaphragm, or female condom, more effective.
6) What Are the Disadvantages of Withdrawal?
Many of us like to weigh the benefits against the risks of using a type of birth control. Now that you're familiar with the benefits, let's look at the possible disadvantages.
There are a few risks to using withdrawal as your only form of birth control. The biggest disadvantage is the risk of performing withdrawal incorrectly.
Withdrawal:
- requires great self-control, experience, and trust
- is not for men who ejaculate prematurely
- is not for men who don't know when to pull out
- is not recommended for teens and sexually inexperienced men because it takes lots of experience before a man can be sure to know when he's going to ejaculate
7) How Do I Practice Withdrawal?
During sex, the man withdraws his p***s from the v****a when he feels he is about to ejaculate, or before he reaches that point. He ejaculates, or comes, outside the v****a, being careful that semen does not spill onto his partner's vulva.
Men who want to use the pull out method need to understand their own sexual response. They need to know when they reach the point in sexual excitement when ejaculation can no longer be stopped or postponed.
There are many other methods available if withdrawal is not right for you. If you need help choosing a method, we're here to help. The staff at your local Planned Parenthood health center can talk with you and help you get the birth control method that's best for you.
-------------------------
Taken from: http://www.birdsandbees.org/BirthControlWhatDoesntWork.htm
Withdrawal Method (Pull-out method):
This method requires that the male withdraw his p***s before ejaculation. The high failure rate of this method shows how difficult it can be to judge the exact moment of ejaculation, as well as having the discipline to withdraw the p***s before doing so. The fluid (pre-c**) that a male's p***s releases upon sexual arousal contains sperm. Additionally, if he has an STI or HIV, the bacteria and viruses that cause these infections may also be presents in the pre-c**. This method is NOT effective in preventing pregnancy, STIs or HIV.
|
 |
 |
|
|
|
|
|
|
|
|
|
|
|
|
 Posted: Sun Jun 28, 2009 10:57 pm Posted: Sun Jun 28, 2009 10:57 pm
Birth Control: Choices and Chances [pamphlet]
[The information in this pamphlet is from the Planned Parenthood Association in BC. I do not claim to own any of this information, and it is not a replacement for professional medical advice from a doctor.]
Birth control has been around for thousands of years. The only 100% effective method of birth control is abstinence. There are many myths out there about birth control methods. These myths do not work as birth control.
All birth control methods work best when used every time and used correctly. Any method will work the best if both partners really want to make it work.
The success of your contraceptive method is less when you or your partner is impaired by alcohol and/or drugs.
Finally, there is the emergency contraceptive pill available for use in situations where you used no protection or where your method failed.
We at Planned Parenthood recognize that religious and family values differ, and encourage you to consider your personal values when making decisions. It is important to choose a method that meets your individual needs.
Saying No, or Continuous Abstinence
This means not allowing sperm near the woman's body below the waist. This keeps the sperm from joining the egg.
- Can be 100% effective if used correctly.
- Helps prevent sexually transmitted infections (STI's).
- No medical or hormonal side effects.
- Some religions endorse abstinence for unmarried people.
- Difficult for many people to abstain from vaginal intercourse for long periods.
- People often forget to protect themselves against pregnancy or STI's when they stop abstaining.
Myths About Preventing Pregnancy
There are dozens of myths about ways in which you can prevent pregnancy. These are just a few examples of common myths, and the truth of reality.
You should know you CAN get pregnant...
- the first time you have intercourse.
It only takes one sperm to fertilize an egg, and it can happen the first time.
- if the girl is on top.
The position of the partners does not affect whether the sperm meet an egg. If ejaculation occurs in or near the v****a, pregnancy can occur.
- if you have intercourse standing up.
- when you're having your period.
Women who have short cycles (21 days in length) can ovulate while they are still having a period.
- if you haven't had a period yet, or haven't had one for months in a row.
Ovulation occurs before a woman has her period and there is no way of knowing if ovulation has occured.
- if you have only one ovary.
Or the biggest myth of all...
- It can't happen to me!
None of these or any other myths about ways of preventing pregnancy are true, regardless of how much you may believe them.
Chances
Making a choice not to use birth control is making a choice to become pregnant or to get a sexually transmitted infection.
Some people use withdrawal (removing the p***s from the v****a before ejaculation), rhythm (counting calander days), and lactation (breast feeding) to prevent pregnancy. Using these methods presents a much higher risk of pregnancy for individuals who practice them. What a pregnancy might mean to a woman should be examined before deciding to use any of these methods.
Choices
The Pill
- must be obtained by a prescription.
- take one pill once a day.
- complete one pill packet each month.
- combination pills contain estrogen and progestin.
- mini pills contain only progestin.
- combination pills prevent release of the egg.
- both types thicken cervical mucus to keep sperm from joining egg.
Effectiveness: 97 - 99% effective - Not effective against STI's (STD's, but referred to as STI's in this pamphlet).
Advantages:
-nothing to put in place before intercourse, more regular periods.
- less menstrual cramping, acne, iron deficiency anemia, premenstrual tension (PMS), rheumatoid arthritis.
- protects against ovarian and endometrial cancers, pelvic inflammatory disease, non-cancerous breast tumors, and ovarian cysts.
- fewer tubal pregnancies.
Possible Problems:
- must be taken daily.
- rare but serious health risks, including blood clots, heart attacks and strokes --> women who are over 35 are at greater risk.
- side effects include temporary irregular bleeding and other discomforts (such as nausea, etc).
Depo Provera
Depo-Provera
- must get by prescription.
- receive a hormone shot in your arm / buttocks every 12 weeks to: prevent release of the egg, thicken the cervical mucus to keep sperm from joining the egg, and prevent a fertilized egg from implanting in the uterus.
Effectiveness: 99.7% effective - Not effective against STI's.
Advantages:
- protects against pregnancy for 12 weeks.
- no daily pill.
- nothing to put in place before intercourse.
- can be used while breastfeeding (6 weeks after delivery).
- can be used by some women who cannot take the Pill.
- protects against cancer of the lining of the uterus, and iron deficiency anemia.
Possible Problems:
- side effects can include irregular bleeding and other discomforts, including weight gain, headaches, depression, and abdominal pain.
- side effects cannot be reversed until medication wears off (up to 12 weeks).
- may cause delay in getting pregnant after shots are stopped.
Norplant (Implant)
- must be obtained by prescription.
- 6 small capsules inserted under the skin of your upper arm.
- capsules constantly release small amounts of hormone that: prevent release of an egg, and thicken the cervical mucus to keep sperm from joining with the egg.
- removal can be done at any time but only by a clinician.
Effectiveness: 99.6% - Not effective against STI's.
Advantages:
- protects against pregnancy for 5 years.
- no daily pill.
- nothing to put in place before intercourse.
- can be used while breastfeeding (6 weeks after delivery).
- can be used by some women who cannot take the Pill.
Possible Problems:
- side effects can include irregular bleeding and other discomforts, including headaches, depression, and weight gain.
- minor medical procedure needed for insertion and removal.
- rarely, infection at insertion site.
IUD
- must be obtained by prescription and inserted by clinician.
- contains copper or hormones that: prevent sperm from joining with the egg (copper), (and/or) prevent fertilized egg from implanting in uterus.
Effectiveness: 97.4% - 99.2% - not effective against STI's.
Advantages:
- nothing to put in place before intercourse.
- cooper IUD's may be left in place for up to 5 years.
- no daily pill.
- no effect on hormone levels in the body.
- IUD's with hormones may reduce menstrual cramps.
Possible Problems:
- temporary increase in cramps.
- heavier and longer periods.
- more than one sexual partner can increase chance of tubal infection, which may lead to sterility.
- rarely, IUD can move out of the uterus, into the abdomen or into the v****a.
Lea Contraceptive
- is a shallow silicon cup.
- must be used with spermicidal jelly.
- can be purchased from a pharmacist without a prescription.
Effectiveness: 86% - 94% - Not effective against STI's.
Advantages:
- no major health concerns.
- no additional gel required within the first 8 hours of use.
- can be left in place up to 48 hours.
- a good alternative for those who have latex allergies.
- one size fits all.
Possible Problems:
- expensive.
- may be difficult to insert.
Diaphram or Cervical Cap
- must be fitted by a clinician.
- is a shallow latex cup (diaphram) or a thimble-shaped latex cap (cervical cup).
- must be used with spermicidal jelly to prevent the sperm from joining with the egg.
Effectiveness: 82 - 94% effective - not effective against STI's.
Advantages:
- no major health concerns
- can last several years, if cared for correctly
Possible problems:
- can be messy
- allergies to latex or spermicide
- cannot use during vaginal bleeding or infection
-- the diaphram has an increased risk of bladder infections
-- the cervical cap can be difficult to use for some women, and can be difficult to fit for some women
Male and Female Condoms
- covers the p***s with a sheath before intercourse (male condom).
- insert into v****a before intercourse (female condom) to prevent the sperm from joining the egg.
- sheath may be made of thin latex (male condom) or polyurethane (female condom). Natural sheep gut condoms are not effective against HIV/STI's.
- condoms come lubricated / non-lubricated.
Effectiveness: 88 - 98% effective - Is effective against STI's (including HIV, the virus that causes AIDS).
To Increase Your Protection:
- also use spermicides.
- do not use oil-based lubricants, like Vaseline, on latex condoms.
- use correctly: put a drop or 2 of water-based lubricant (like K-Y jelly) in tip of condom. Place rolled condom on tip of hard p***s. Leave a half-inch space at tip. Pull back foreskin and roll condom down over p***s - smooth out any air bubbles.
- hold condom against p***s to withdraw.
Advantages:
- easy to buy in drugstores, supermarkets, etc.
- can help relieve premature ejaculation.
- can be put on as part of sex play.
Possible problems:
- allergies.
- loss of sensation.
- breakage.
Vaginal Spermicides
- made of chemicals that immobilize or kill sperm.
- create a barrier that sperm cannot penetrate.
- come as contraceptive foams, gels, film, suppositories and in sponges.
- can be purchased in pharmacies.
- are most effective when used with sponges.
Contraceptive Sponges
- is a polyurethane foam filled with F5 Gel (2 low dose spermicides).
- fits into the v****a easily.
- insert just prior or up to 1 hour before sex.
- F5 Gel covers walls of v****a and is released during intercourse.
- can be left in for 12 hours.
- can be used with a condom for extra protection.
Sterilization: Male and Female
- an irreversible method of birth control.
- procedure must be done by a doctor.
- female sterilization (tubal litigation) involves cutting the fallopian tubes to prevent an egg from traveling down to the uterus.
- male sterilization (vasectomy) involves tying off the vas deferens which carry the sperm to the glands containing seminal fluid.
Effectiveness: 99.9% effective - Not effective against STI's.
Considerations:
- counselling important because procedure usually cannot be reversed.
Emergency Contraceptive Pill
- a hormonal method using 4 pills.
- must be obtained by prescription.
- must be taken within 72 hours of having an episode of unprotected sex.
- changes the transport time of the egg moving down the fallopian tubes, or makes the environment unsuitable for implantation.
Effectiveness: 96% effective - Not effective against STI's.
Possible Problems:
- may make user very nauseated.
- may delay onset of menstrual period for up to 3 weeks.
Using condoms will all of the above mentioned methods will help to protect against sexually transmitted infections (STI's).
Planned Parenthood Clinics Are Available in the Following Areas:
[Applies to BC, Canada only]
- Abbotsford/Matsqui
- Burnaby
- Campbell River
- Chilliwack
- Comox Valley
- Coquitlam
- Cranbrook
- Kelowna
- Ladysmith
- Langley
- Maple Ridge
- Mission
- Nakusp
- Nanaimo/Malaspina
- Nelson
- New Westminster
- North Vancouver
- Port Alberni
- Port Coquitlam
- Powell River
- Salmon Arm
- Salt Spring Island
- Smithers
- Sunshine Coast
- Surrey/Delta/White Rock
- Terrace
- Vancouver
- Vernon/Lumby
- Whistler
|
 |
 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
 Posted: Mon Jun 29, 2009 12:04 am Posted: Mon Jun 29, 2009 12:04 am
Things That Interfere With Your Birth ControlTaken from: http://www.suite101.com/article.cfm/birth_control/92276 (Thank you mythrilmercury!) I have been asked this question in one form or another several times. Women need to know that the birth control form they have chosen will be effective, but depending on the other medications and herbs that you use, this may not the case. Learn what drugs and herbs you should avoid while taking hormonal contraception, and why it is important to tell your doctor about your birth control choice. Usually I am asked about diet pills and breast enhancement pills and if they will decrease the effectiveness of the pill. Unfortunately my answer is usually "I don't know, what are the ingredients?" Dependent on what is them, that will decide if it will affect hormonal forms of birth control. Hormonal forms of birth control include the pill, mini-pill, Norplant, Depo-Provera, Ortho Evra (the patch), Lunelle, the progesterone IUD, and NuvaRing. There are many different medications and herbs that can lower the effectiveness of these forms of contraception. HERBS Herbs to avoid while using hormonal birth control include St. John's Wort, Vitex (chasteberry), Red Clover, Black and Blue Cohosh, Fennel, Hops, Dong Quai, Wild Yam, and Licorice. There could be many other herbs that interfere with the effectiveness of birth control, but because few studies have been done, it is not known which ones do this. Most of the herbs listed interfere because of their properties. All of them, except for the Licorice and St. John's Wort, contain hormones (mostly estrogen) and can interfere with hormonal birth control by providing too much, or by causing the body to try to 'correct' any hormonal imbalance present. St. John's Wort can cause irregular bleeding (bleeding between periods). Because of this it is thought to reduce the effectiveness of hormonal forms of birth control. How it might do this is not known. Licorice can increase blood pressure and lower potassium levels when taken by women that are using hormonal forms of birth control. Because of the seriousness of these, licorice should be avoided while using hormonal contraceptives. Any herbs that are known for their fertility enhancing properties should be avoided while taking hormonal forms of birth control. ANTIBIOTICS Some antibiotics will cause a decrease in the effectiveness of hormonal birth control, so when using these drugs to treat infections, a non-hormonal back up method must be used. Most of the antibiotics are in the Penicillin and Tetracycline families. These include, but are in no way limited to; Amoxicillin, Ampicillin, Penicillin, Demeclocycline, Doxycycline, and Tetracycline. The antiviral drug Griseofulvin and the antituberculosis drug Rifampin can also cause hormonal forms of birth control to become less effective. OTHER MEDICATIONS Some of the other medications that can decrease the effectiveness of hormonal forms of birth control are barbiturates, HIV drugs, and epilepsy controlling medications. There are several types of all of these, and either taking one that will not affect your birth control method, or changing your method if there is no other option would be the best thing to do. Some of the barbiturates include Secobarbital, Phenobarbital, Amobarbital and some others. The two HIV drugs that I found that can interfere with birth control are Nelfinavir and Ritonavir; there could easily be others. The epilepsy drugs that decrease the effectiveness of birth control include Tegretol, Dilantin, Luminal, Mysoline, and Topamax. The epilepsy drugs that increase the hormone levels when taken with birth control are Depakote, and Felbato. There are two epilepsy drugs that do not affect hormonal birth control, Neurontin and Lamictal. WHAT YOU CAN DO One of the first things you should do is to tell your doctor or health care provider about all medications that you are taking (including birth control). This is the first thing you can do to help guard against birth control failure. The next thing you should do is to ask both your doctor and your pharmacist about any drug interactions. Before you get a prescription filled, double check that it will not interfere with your birth control method. RESOURCES http://www.drkoop.com http://www.webmd.com http://www.healthandage.com/html/res/com
|
 |
 |
|
|
|
|
|
|
|
|
|
|
|
|
 Posted: Mon Jun 29, 2009 12:31 am Posted: Mon Jun 29, 2009 12:31 am
Links and Resources[I'm sorry that most of these phone numbers apply to British Columbians in Canada only. Hopefully some of the websites will still be useful for people outside of Canada. sweatdrop ]STD ResourceFor more information on preventing and managing sexually transmitted diseases, please visit STDresource.com. www.STDResource.com - BC's information source for sexually transmitted diseases. Opt: Options for Sexual Health- Birth control counselling and supplies - Reproductive health and human sexuality counselling and education - Examinations by doctors and nurses - Pregnancy tests, counselling and referrals - Emergency contraceptives available www.optionsforsexualhealth.org ECP: Emergency Contraceptive PillThe emergency contraceptive pill can help prevent pregnancy if taken within 72 hours of unprotected sex (not just the morning after). Call the ECP Hotline for a list of providers in your area. Now available directly from participating pharmacists. 1-888-Not-2-Late (toll-free) www.not-2-late.com Planned Parenthood BC- Confidential information and referrals - Birth control - Pregnancy options - Emergency contraception - Sexually transmitted infections and HIV 1-800-Sex-Sense (1-800-739-7367) (604) 731-7803 (in the Lower Mainland of BC) www.factsoflifeline.com Kelowna Women's ShelterEmergency Line: (250) 763-1040 http://kws.shelternet.caWon't Get Weird - Sex SenseTalk about sex and some people get weird. We won't. www.wontgetweird.com 1-800-Sex-Sense (1-800-739-7367) (604) 731-7803 [Lower Mainland only]
|
 |
 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
 Posted: Mon Jun 29, 2009 12:34 am Posted: Mon Jun 29, 2009 12:34 am
Birth Control and Weight GainTaken from: http://www.wdxcyber.com/ncontr11.htm"I have been taking birth control pills for about six months now. I am thrilled at the idea of not becoming pregnant, however, my problem is tremendous weight gain as a result of water retention. I have experienced no increased appetite, however my breasts are a full cup size larger and I feel that I have an added layer onto my body that makes me very uncomfortable. Is there anything that can be done about this problem?" - Anon Before we know if there is any way we can treat weight gain associated with oral contraceptives, we need to know if birth control pills cause fluid retention and by what mechanism, do they cause increased appetite and how, and do they cause temporary or long term weight gain by those or any other mechanisms? With studies of recent low dose oral contraceptives, the whole premise as to whether there is any change in weight at all with beginning oral contraceptives is in question (1). This and other studies indicate that, on the average, women do not gain weight because of the pills. Remember this means that if 5-10% of women report weight gain when starting oral contraceptives, there is an identical 5-10% of women who gain weight even though they did not get active birth control pills. In other words the weight gain with pills was coincidental but not a cause and effect. We know from older birth control pill studies, however, that weight gain was a problem both from fluid retention and from more fat deposition so we need to look at what was learned from those studies because those factors may be active in some women who are sensitive to them even at today's low pill hormone doses. Do most women gain weight when starting on oral contraceptives and if so how much? For the most part, older studies using higher dose pills tend to show an average of about 5 lb weight gain using pills. One study looked at adolescents who were using DeproProvera® (DMPA) for contraception and compared them to other teens using birth control pills (1). They found that after one year of contraception, the average weight gain was 6.6 lbs (3.0 kg) in the adolescents using shots (DMPA) and 5.3 lbs (2.4 kg) when using oral contraceptives. More importantly, only 7% of pill users gained more than 10% of their body weight while 25% of the DepoProvera® users gained more than 10%. If you just look at the average weight gain of 6.6 lbs vs 5.3 lbs, you would conclude that DMPA had only a slightly higher weight gain than pills. The fact that these averages include 18% more woman who gained greater than 10% of body weight can be hidden by average weight changes. Thus DepoProvera® has a greater side effect of weight gain than oral contraceptives. In another study with a fairly high dose pill (50 mcgm) from 20 years ago, investigators found an 11.4% weight increase of over 4.4 lbs (2.0 kg) but also a 14.3% incidence of over a 4.4 lbs weight loss on the same pill (1). In other words there was just as much weight loss as weight gain. This finding could be interpreted as the pills cause no overall weight change in woman on the average, but an alternative explanation is that some women get nauseated from pills and have a net weight loss while the others who did not get nauseated gained a substantial amount of weight. Do oral contraceptives cause water retention and how much? Estrogen in high doses is known to cause weight gain especially that due to fluid retention (1). The more estrogen there is in a pill, the more tendency to gain weight such that a 50 mcgm pill will result in more weight gain than a 35 mcgm pill (1). The mechanism of action is probably direct stimulation by the estrogen in pills of kidney substances called renin-angiotensin that cause water retention. The water retention then causes sodium (salt) retention. A lower estrogen level pill, e.g., 20 mcgm, will help reduce weight gain due to fluid retention.This was confirmed in a more recent study with 30 mcgm pills in which there was essentially no difference in weight gain or weight loss between the placebo group and the oral contraceptive group (1). Again, however, 30% of these women had a weight gain of more than 1 lb but the net result was the same in the control group. Those who did have weight gain had increased fat but no difference in fluid retention amounts indicating that fluid weight gain may be less of a problem with the newer, lower estrogen pills. Do birth control pills stimulate your appetite? There have been reports through the years, especially with the older, higher dose pills, of adverse effects on insulin resistance. Even recent studies seem to indicate that current pills can raise insulin levels. Insulin resistance is a condition in which insulin levels rise in response to carbohydrates and drive all energy into the fat cells and essentially prevent weight loss even with dieting. Not all women are susceptible to insulin resistance and thus not all women gain weight using oral contraceptives. Those that have a tendency to abnormal glucose metabolism, however may be the ones who gain weight. If a woman gains weight upon starting oral contraceptives and there are not other explanations, she should be checked out for possible insulin resistance. Are there other mechanisms by which pills cause weight gain? In one study of pills, a formulation containing desogestrel as the progestin and slightly less estrogen had significantly less weight gain when compared to a pill containing norethindrone (Ortho Novum 7/7/7®) (1). This may imply that the specific progestin has a role in weight gain, possibly through a lesser degree of insulin resistance. Or it could be the combination of lower estrogen and the specific progestin but in any case, there was less weight gain. Currently marketed pills with desogestrel as the progestin are Desogen® and Ortho-Cept®. What can you do if you have weight gain on the pills? Using the lowest possible estrogen containing birth control pill should minimize weight gain and swelling from water retention. Current 20 mcgm pills which are the lowest estrogen doses available are: - Alesse® - Levlite® - Loestrin-Fe® - Mircette® If you are not taking one of the lowest dose pills, ask your physician or health care provider to switch you to one of the lowest dose pills, especially if you are having any weight gain or fluid retention symptoms. Any weight gain after starting pills of more than 5% of body weight may be a signal of a woman's tendency toward insulin resistance or abnormal glucose metabolism. With this amount of weight gain associated with an oral contraceptive, I would suggest the woman be evaluated for possible insulin resistance. If this condition is present, she will have to adopt a low carbohydrate diet. Simple sugars in any amount and high carbohydrate only snacks or meals will negate all other dieting efforts on a daily basis and frustrate any long term ability at weight control. ~ Taken from: http://www.fin.org/mqa_bcp_weight.htmlQ#1: I am a 23 year old female who has been on the birth control pill since I was 17 years old. I started out using Desogen and for about the past five years have been on Orth Tri-Cyclen. I have switched insurance carriers and my Insurance will no longer cover this pill. I am not always sexually active, I am trying to loose the weight I gained from college (about 30 pounds) and have excess facial hair. My doctor has tested me for that Ovarian syndrom, but found it out to be not a problem that I had. I am wondering a few things. First, if I go off the pill will I be able to loose weight easier or do you recomend a pill for me that will help control my weight & facial hair as well as minimal acne? It is not necessary for me to be on the pill, although it does help control irregualr periods. Will Ortho-novum 777, Tripasil or Tri-norinyl help with any of these problems? I appreciate all your help and an answer as soon as you can get back to me. 10/04/2000 A: Many studies have been done around the world trying to decide if oral contraceptives cause weight gain. In theory they could. But the studies have either been equivocal or show no association between the pill and weight gain. But everyone is different. The only way to know for sure in any one situation is to stop the pill for three months and see how it goes. An IUD or other method would protect you during this time. You certainly have many of the symptoms of polycystic ovary syndrome. It is not always easy to diagnose and unless you have had extensive or repeat tests the question may still be unanswered. And it does make a big difference in what you might want to do. I would consider seeing an endocrinologist who likes to work with these problems. I think that is more important than just jumping to another pill. If you and your doctor are really satisfied that you don't have polycystic ovaries then I still would treat with a pill that tends to block the androgen excess that may be contributing to your weight and and excess facial hair problems. (But this recommendation would not be the same for polycystic ovaries.) Mircette is a pill that has the same progestin that was in the Desogen you were taking. And this progestin has been shown to be the best to depress the androgen effect on hair growth. Mircette has less estrogen and the less hormone the less likely for weight gain--in theory. Namaste. Dr. JJ Q#2: I am a 25 yr. old woman. I had been on Ortho-cept for 4 1/2 yrs, and recently was switched to Mircette due to inability to lose weight, excessive moodiness etc. I have been on Mircette for 4 months and despite my healthy lifestyle (workout each night-30 min. cardio, 30 min light weight trainning) I have gained 11 lbs. in less than two months......I AM HORRIFIED! I used to be VERY heavy and lost about 65 lbs., so to someone like me this out of the blue 11 lbs. is a nightmare. I'm getting married in 10 months and need to be in a gown, that has been sized already!!!! I am now blaming my new pill, so I have decided to go off mircette and keep up my exercise and low fat diet to see what happens. What side effects can I expect by going off the pill after almost 5 yrs. now? I am hoping for less of a barrier to weight loss, but I've seen some horror stories on other sites about jitteriness, nausea, nightsweats.....any info would be greatly appreciated. 08/27/2000 A: Almost all of the studies done to prove or disprove weight gain, with the pill, have shown no effect for most people. As many loose weight as gain. But there certainly can be individual sensitivities that can account for your weight gain. And if you are sure it is just not anxiety related eating, etc. associated with wedding "stuff" such as extra lunches, showers, etc. then the pill can be your problem. Switching to a different pill is not likely to help. I would recommend going off the pill and considering an IUD for contraception. Congratulations and best wishes for a long life. Today is my anniversary and I strongly recommend married life. Namaste. Dr. JJ Q#3: I am 25 years old and have never been on "the pill" before. My periods have a tendency to be late (my last period was 15 days late), and I frequently have heavy bleeding and cramps. After my last horrible period I decided that I would go on the pill. My doctor prescribed Mircette. I forgot to ask him a couple of questions: 1. Will I likely gain weight? I just recently lost 35 pounds and would hate to gain it back, and 2. I am waiting for my next period to start to start the pill pack. I will be using the Sunday start. How long should I use a secondary method of birth control after I start taking the pills? Thanks! A: Weight gain is possible with any oral contraceptive. Mircette would be no worse nor better than any other low dose pill in this regard. You will just have to see how it goes. Most people don't have much trouble on the low dose pills like Mircette. The number of unwanted pregnancies is highest during the first couple of months one is on the pill. This is due to errors in how patients remember to take the pill, not in the way the pill works. For this reason some physicians recommend a back up method the first month or two. But if you take your pills every day within a couple hours from when you took the one the day before you should be fine from the get-go! Namaste. Dr. JJ Q#4: I've been off and on Ortho-Tricyclen for the last 2 years. I am 23 years old, 5'2 and about 115 pounds. I went off BCP's around 5/1999 and I suffered through a traumatic experience where I went down to about 100 pounds. I got pregnant 10/1999, and I decided to get back on the pill. I exercise vigorously for about 3-4days a week and 2-3 hours each time (including 45 minutes of cardiovascular activity during that time). I feel as though I maintain a healthy, wholesome diet and I usually don't eat anything but fruits after 6pm. I've gained about 10 pounds since I've gone back on the pill, and I would like to know if it is attributed to the BCP's. A: Unless you have additional information that would suggest otherwise, it wounds like the pill is associated with your weight gain. I could not tell from your note whether that was bad or good?! The weight might stabilize and not continue. If that is OK then you have to decide if that is a problem. If the weight continues then the pill may not be for you. You are on a pretty low dose pill. I doubt switching would make much difference. How about an IUD? Namaste. Dr. JJ Q#5: I'm a 16 year old female and have been on birth control pills for the past 3 months. I'm on them due to acne, nothing sex related. I went off them just about a month ago because I couldn't handle the fact I was gaining so much weight. In one months time being off them I lost 8 pounds. I returned to the dermatologist today and decided to start Accutane, another acne medication. but in order to do so I have to get on birth control pills again. my acne isn't bad at all and I'm thrilled to know that after taking accutane I wont have to touch acne medicine again. But I can't go through the fact of gaining so much weight and feeling so moody and sick. I know I'm young and still growing but is there anything to prevent so much weight gain? I just don't feel happy due to it. and I'm very active in soccer and sports therefore it increases the water intake. anything you can tell me about this would be of great help. Thanks! (7/19/00) A: Not much in life is simple, is it? All oral contraceptives can cause weight gain. It sounds like your weight gain was more fluid retention. That is good because that corrects itself pretty easily if you don't stay on the pills. And the side effects of fluid retention and weight gain are often related to the types and amounts of each hormone in the "pill". When you go back on the pills you might try a different pill that is not quite so strong. The ones used for acne usually have more estrogen and for just birth control you might get by with a milder one with less estrogen and therefore have fewer side effects. You and your doctor can discuss this. I am a little disturbed to hear you say that, "my acne isn't bad at all" and after taking Accutane you will never have to touch acne medicine again. Accutane is a powerful medication with significant side effects and is usually reserved for someone who has pretty bad acne that is not well controlled with other methods. It works very well and usually young people have no permanent side effects. But, it does not always stop all the problems for everyone. Namaste. Dr. JJ Q#6: I take Ortho-cept. I take the pill at night and when I wake up in the morning I feel a little sick to my stomach. When I eat something I feel better. I've been taking this pill for two months now, and my appetite has increased a lot and I never feel full. What's up with that, am I taking the wrong pill or will my increase appetite go away? Any other pill suggestions or should wait and see what happens? (07/06/00) A: Nausea and weight gain are not uncommon problems with oral contraceptives. We often ask people to stay on a pill for three months before deciding whether or not to change due to side effects. But the weight gain is not likely to change after three months. Your pill, Ortho-Cept is moderately high in hormone effects compared to some others. Some pills with less hormone effects that may work better for you would include: Aleese, Brevicon, Modicon, and Tri-Norinyl. I would try one of these and see what you think. If weight gain continues to be a major issue how about an IUD? Namaste. Dr. JJ Q#7: I am 19 and have been on 28-Ortho Tri-cyclen for 3 months now. I have noticed a significant difference in my skin, but my weight is now a major issue. I have gained a few pounds since being on the pill. I have also noticed my appetite growing. Is this normal? Will I continue to gain weight if I remain on this pill or is my body just still adjusting to the pill? 07/19/00 A: Weight gain is associated with all oral contraceptives and can be from either of the hormones. When that is a problem we use the lowest possible dose that will do the job or regulating the periods. You did not mention the name of your pill but it probably doesn't make a lot of difference because individual variation is hard to predict. If you have an increased appetite since being on the pill it is likely to continue. But each person is special and you will just have to wait and see. You might ask your doctor if there is a milder pill that might still work for you. Namaste. Dr. JJ Q#8: First let me say that I'm so glad I found your web site. Very informative! I am 46 years old and suffering from severe hormonal swing symptoms for over a year when I discovered that I suffered from hypothyroidism (levels were at "95" a year ago but under control currently at 1.62). I suffer from every symptom from mood swings, crying jags, irritability, weight gain & bloating to tingling of lips (Low blood sugar) insomnia, anxiety, severe fatigue..... I have tried several types of HRT since this past Feb including Premarin, Estrace, & most recently climara patch with progesterone cream. Well, I feel somewhat better (especially with the progesterone cream) but still suffer from fatigue & insomnia, concentration, focusing and bloating & weight gain. I also get dizzy when off the progesterone cream on estrogen only. I've read about treating peri symptoms with low dose birth control pills and will be starting Ovcon35 this Sunday. I realize this is a higher estrogen lower progestin pill. There seems to be more push (from what I've read lately) for Loestrin/20 or Alesse. I think the majority of my symptoms are from estrogen dominance but not sure. The one thing I notice is that I am more fatigued on the patch (.50) vs. Estrace at 1.0. I've had my estridiol & progesterone levels tested (saliva). Estradiol 0.50 Progesterone 0.02 - both very low. Do you think I should start on Ovcon35 (a higher estrogen that the Loestrin?) Hope you can help. Thank you. A: Since your thyroid level was off so much you could still be settling out from low thyroid and some of your symptoms may change for the better in the next six months, after being on the correct thyroid medication a little longer. Many women are being kept on low dose oral contraceptives right up to menopause. In addition to controlling irregular periods the oral contraceptives can reduce hot flashes, decrease mood swings, and may lower the risk of ovarian and endometrial cancer. The effects on breast cancer may be negative and if you are at increased risk for that you may not want to take the chance. The pill also increases the risk of blood clots in the legs and should not be taken by women over 35 who smoke, have uncontrolled high blood pressure, or a history of blood clots or stroke. Checking hormone levels is probably a waste of time because these are not very reliable. The problem with hormone replacement at your age is determining when you are really into menopause and don't need birth control any more. The way we do that is to take a blood sample on the 7th. day of the pill-free interval and check for an estradiol level less than 25 picograms/ml and an FSH/LH (follicle stimulating hormone/leutinizing hormone) ratio greater than 1. When you have reached menopause then you can go on lower dose pills that are hormone replacement levels and not oral contraceptive strength. I think you are trying too many complicated schemes and should just go on the pill for three months and see how you feel. Your choice of Ovcon 35 seems like a reasonable choice. After three months on the pill you can tell better which symptoms you still have and make a different choice more reasonable. And you may need an antidepressant or some other treatment besides oral contraceptives. And don't forget that lifestyle changes can be of great help, also. Namaste. Dr. JJ Q#9: I have been going to the gym and walking all of the time. I have also been eating healthy. I went from being 130 to 115. at the time my were always 28-29 days apart but they began to be like 35=40 days apart. I went to my doctor and she said it was due to my weight change. that day I was put on orthtricyclen. not to regulate my periods but because I am sexually active. so i wasnt sure if the pill would regulate my periods or not. since I have been on it (almost finished with the first pack) I have gained 4 pounds back. A: Weight loss associated with strenuous exercise is a well known cause of periods stopping all together. Under these circumstance the right pill probably would cause you to have a period. But it is not necessary to have periods. And not having a period does not increase the risk of getting pregnant. Thanks for the feed-back. Namaste. Dr. JJ
|
 |
 |
|
|
|
|
|
|
|
|
 |
|
|
|
|
|
|